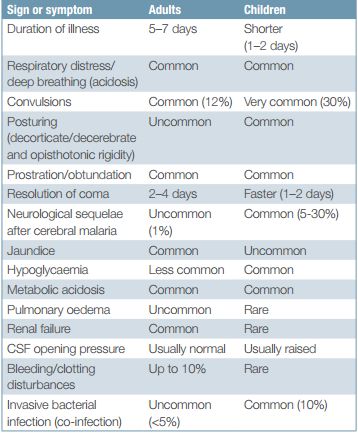
Criteria for Severe and Complicated Malaria
Positive peripheral blood smear for P.falciparum + ≥1 of the CHAPLINS (Mnemonic)
- Convulsions: >2 in 24 hour
- Cerebral edema (Consciousness impaired)
- Hypoglycemia (glucose <40 mg/dl)
- Hemorrhage (DIC)
- Hemoglobinuria (Black water fever)
- Anemia (hemoglobin <5 gm/dl or PCV <15% in children; hemoglobin <7 gm/dl or PCV <20% in adults)
- Pulmonary edema or ARDS
- Lactic acidosis (pH <7.25, lactate >5 mmol/l, bicarbonate <15 mmol/l)
- Infection (>5% erythrocytes infested)
- Icterus (Bilirubin >3 gm/dl)
- Necrosis i.e. ATN (Serum creatinine >3 mg/dl, oliguria)
- Shock (SBP <80 mmHg in adults; SBP <50 mmHg in children)
Where microscopy is unavailable or not feasible, Rapid Diagnostic Test (RDT) using HRP-2 must be used. Frequent monitoring of parasitemia (e.g. every 12 hour) is important during the first 2-3 days of treatment in order to monitor the parasite response during the treatment. RDTs for detecting HRP-2 cannot be used for this purpose because it can remain positive for upto 4 weeks after clearance of parasitemia.
Antimalaria Drugs for Severe Malaria
Antimalaria drugs should be given:
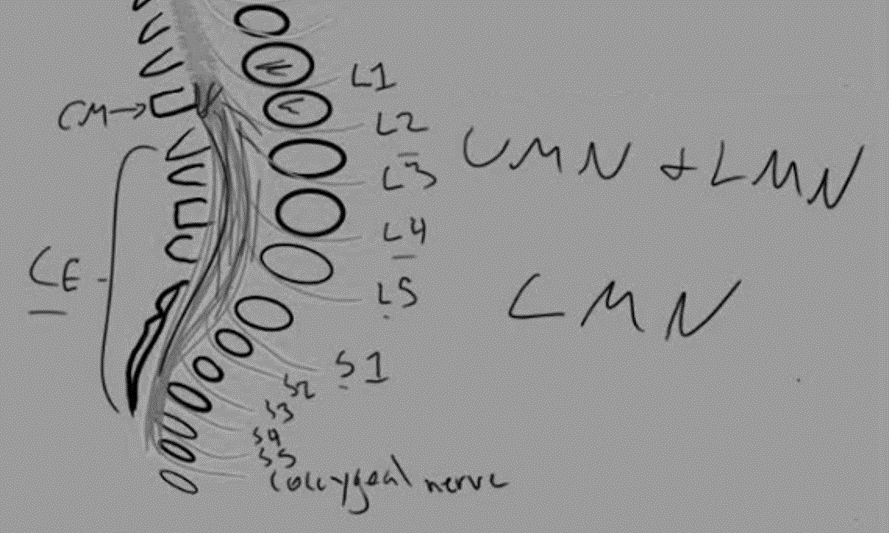
- Parenterally for minimum 24 hours (intramuscular injections must not be given in buttocks due to risk of sciatic nerve injury)
- Then, replaced by oral medications as soon as it is tolerable
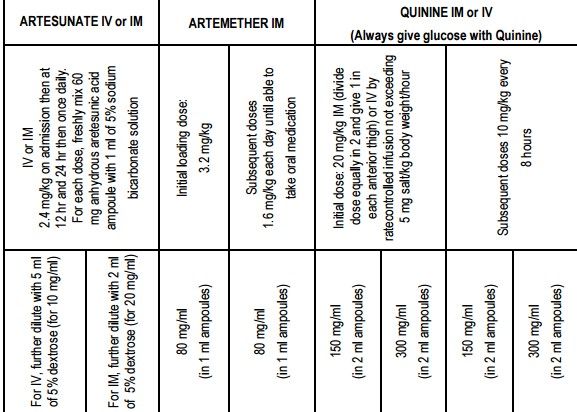
Drug of choice: Artesunate IV or IM
Alternatives: Arthemeter IM, Quinine IV or IM
Besides, antimalarial drugs – patient must be treated side by side for seizure, hypoglycemia, hyperpyrexia, DIC, renal failure, acute pulmonary edema, etc.
Start broad-spectrum antibiotics along with antimalarials in following conditions:
- Meningitis cannot be ruled out in case of altered sensorium.
- Suspected bacterial co-infection: hypotension, pneumonia.
Reference: Management of Severe Malaria – A practical Handbook 3rd edition byWHO