ANATOMY OF SPLEEN
- Location: Left hypochondrium
- Rule of odds (1,3,5,7,9-11):
- 1 inch thick
- 3 inches broad
- 5 inches long
- 7 ounces weight
- underlies 9-11 ribs
- Position: obliquely along long axis of 10th rib; directed downward, forward and laterally
- Arterial supply: Splenic artery from celiac trunk
- Venous drainage: Splenic vein → Portal vein
- Lymphatic drainage: Celiac (Para-aortic) nodes
- Nerve supply: Sympathetic from celiac plexus
Histologically:
- Red pulp: sinuses lined by endothelial macrophages and cords (spaces)
- White pulp: structure similar to lymphoid follicles
FUNCTIONS OF SPLEEN
Spleen is the largest lymphoid organ organ and serves following functions –
- Red pulp: Removal of senescent and defective RBCs (mechanism: hypoxia, low pH and low glucose)
- White pulp: Synthesis of antibodies
- Removal of antibody-coated bacteria and anti-body coated blood cells from circulation
- Extramedullary hematopoiesis
- Blood pooling
An increase in these normal functions may result in splenomegaly
EXAMINATION OF SPLEEN
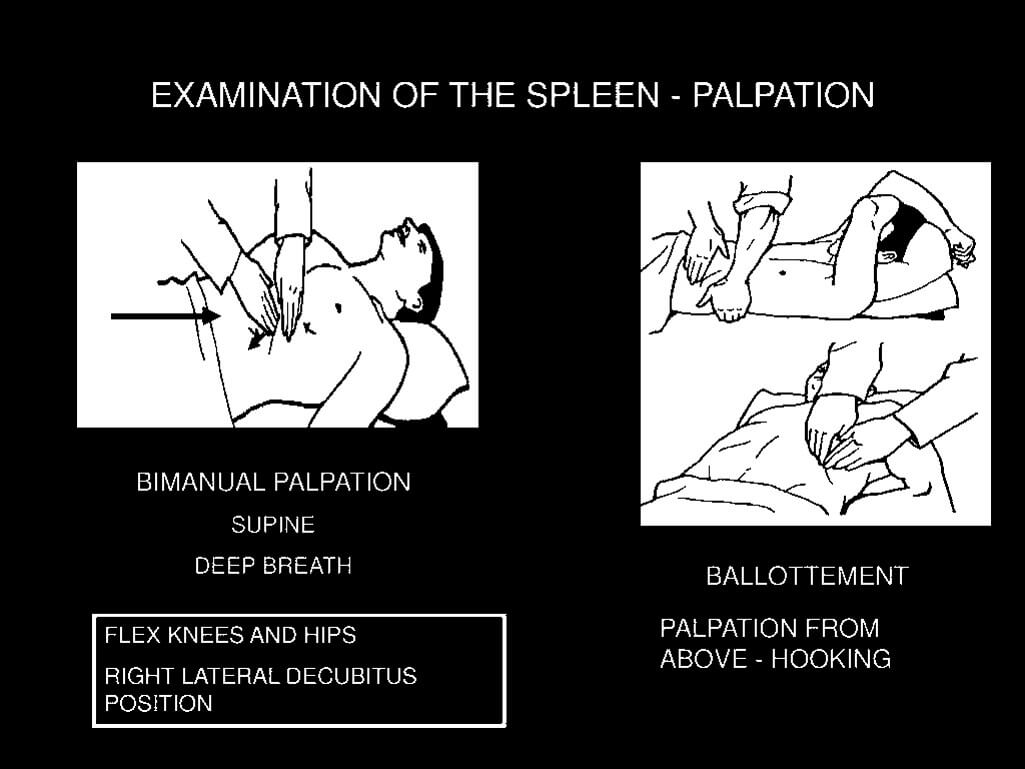
1. Palpation:
- Right hand: Keep hand still and ask patient to take a deep breath through the mouth to feel spleen edge being displaced downwards. Move hand up diagonally from right iliac fossa, towards left upper quadrant on expiration.
- Left hand: Place the hand around patient’s lower ribs and approach costal margin to pull spleen forward
If history suggest splenomegaly but is not palpable: Roll the patient on to the right lateral position with flexion of left hip and knee and examine as before.
Splenomegaly: Abnormal enlargement of Spleen
If ascites is gross: Use dipping method to palpate the spleen
2. Percussion:
- Examine the spleen with the patient holding the breath during full inspiration; percuss both below and then above the left costal margin
- Percuss from resonance to dullness
Castell’s sign: With the patient supine, percussion in the lowest intercostal space in the anterior axillary line (8th or 9th) produces a resonant note if the spleen is normal in size. This is true during expiration or full inspiration. A dull percussion note on full inspiration suggests splenomegaly.
MECHANISMS OF SPLENOMEGALY
1. Work hypertrophy
- Reticuloendothelial system hyperplasia (Removal of defective erythrocytes)
- Immune hyperplasia (Response to infection or disordered immunoregulation)
- Extramedullary hematopoiesis (Bone marrow disorder)
2. Infiltration
- Acellular deposition: Metabolic disorders
- Cellular deposition: Neoplasia
3. Passive congestion
CAUSES OF SPLENOMEGALY
Mnemonic: CHIMPS
- Congestive: Portal hypertension (Cirrhosis, Hepatic/Splenic/Portal vein occlusion), Cardiac (CHF, Constrictive pericarditis)
- Hematologic: Neoplastic (Lymphomas, Leukemias, Myeloproliferative disorders), Non-neoplastic (Megaloblastic anemia, Hemoglobinopathies, Autoimmune hemolytic anemias)
- Infective: Subacute Bacterial Endocarditis (SBE), Brucellosis, TB, Salmonella, Septic shock, Infectious mononucleosis, Hepatitis, Cytomegalovirus (CMV), Histoplasmosis, Malaria, Leishmaniasis, Schistosomiasis, Trypanosomiasis
- Inflammatory: Felty’s syndrome, SLE, Rheumatoid arthritis, Sarcoidosis
- Metabolic-infiltrative: Gaucher’s disease, Niemann-Pick’s syndrome, Amyloidosis
- Miscellaneous: Cyst, abscess, cavernous hemangiomas
- Primary hypersplenism: Dacie’s syndrome (Splenomegaly of unknown cause + Pancytopenia)
- Splenic cyst or hamartoma
Felty’s syndrome: A triad of Rheumatoid arthritis, Splenomegaly and Neutropenia
Hypersplenism: It is the splenic hyperactivity with increased blood cell destruction. Diagnostic criteria are:
- Splenomegaly
- Pancytopenia
- Normal bone marrow (Primary) or Hypercellular bone marrow (secondary)
- Reversibility by splenectomy
Banti’s disease: Congestive splenomegaly with hypersplenism occuring in cirrhosis and portal hypertension
CLINICAL APPROACH TO SPLENOMEGALY
A) History:
1. Suggestive of splenomegaly:
- Pain and a heavy sensation in LUQ radiating to back
- Radiation to left shoulder tip in splenic infarction
- Early satiety in massive splenomegaly
2. Suggestive of associated disease:
- B symptoms i.e. Fever, night sweats, or weight loss (Neoplastic, SBE and other infections)
- Bone pain (AML, Sickle cell disease, Gaucher’s disease)
- Fatigue, dyspnea, bruising and/or petechiae (Hemolytic)
- Joint pains (RA, SLE)
- Pruritus (Hodgkin lymphoma, Polycythemia)
- Epigastric or generalized abdominal pain (Splenic vein thrombosis eg. Pancreatitis)
- Cough and dyspnea (Sarcoidosis)
- History of alcoholism, liver disease (Liver cirrhosis)
- History of Pancreatitis (Splenic vein thrombosis)
- Personal or family history of hemoglobinopathy, lysosomal storage disorder, rheumatoid arthritis
- History of neonatal umbilical vein sepsis (Portal vein thrombosis)
- Recent infections including malaria
- History of recent dental work or blood transfusions (SBE)
- Recent abdominal trauma
B) Physical examination:
1. Inspection: Fullness in LUQ that descends on inspiration (massive splenomegaly)
2. Palpation: Spleen is not normally palpable (palpable when 2-3 times enlarged). Enlargement takes place in a superior and posterior direction before it becomes palpable subcostally. A palpable spleen must be reported in following points:
- Degree of enlargement: Measured below from the left costal margin along the splenic axis in centimeters/inches or number of fingers
- Splenic notch: Felt on its lower medial border
- Margin: Usually sharp
- Consistency: Soft, firm or hard
- Tenderness: Tender or non-tender
- Surface: Smooth or irregular
- Movement with respiration: Always moves downwards and medially with respiration
- Fingers insinuation: cannot get between spleen and ribs
- Palpable splenic rub: Present or not
A palpable spleen is distinguished from palpable left kidney mass by:
- Not bimanually palpable and not ballotable
- Upper border cannot be felt
- Notch on lower medial border
- Fingers cannot get between spleen and ribs
- Dull on percussion
Normal sized spleen may be palpable in:
- Chronic Emphysema
- Low diaphragm
3. Auscultation: Venous hum or a friction rub may be heard
4. Percussion: Palpation is confirmed by dullness as spleen is dull to percussion
5. Other relevant findings in Physical Examination:
a. Skin:
- Pallor: Chronic malaria, Chronic kala-azar, Leukemia, Lymphomas, Cirrhosis, Hemolytic anemia, Hypersplenism
- Icterus: Hemolysis (Hemolytic anemias, Acute malaria, Lymphoma), Budd-Chiari syndrome (Hepatic vein obstruction), Chronic liver disease
- Periorbital purpura: Amyloidosis
- Plethora: Polycythemia vera
- Skin infiltration and masses: AML or ALL
- Butterfly rash: SLE
- Janeway lesion: SBE
- Erythema nodosum, lupus pernio: Sarcoidosis
- Spider naevi and palmar erythema: Portal HTN due to chronic liver disease
- Hemorrhagic spots: Acute leukemia, SBE, SLE, ITP, Felty’s syndrome, Blast crisis of CML or CLL
b. Lymphadenopathy:
- Autoimmune disorders: RA, Felty’s syndrome, SLE, Sarcoidosis
- Infection: Infectious Mononucleosis, AIDS, Toxoplasmosis, CMV, Disseminated TB
- Neoplasm: Lymphomas and Leukemias
c. Fever
- Infections: Malaria, Kala-azar, Enteric fever, SBE, Miliary TB, Acute viral hepatitis
- Neoplasm: Acute leukemias, CML, Lymphoma
- Collagen vascular diseases
d. Eyes and ENT
- Suffused conjunctiva: Polycythmia vera
- Fundoscopy: Roth spots (SBE), Choroidal tubercle (Miliary TB)
- Pharyngitis: EBV infection
- Macroglossia, Jugula vein distension or Periorbital edema: Amyloidosis
- Mongoloid facies: Thalassemia
e. Cardiac examination:
- New or changing murmurs: SBE
f. Extremities:
- Digital ischemia/gangrene or thrombosis: Essential thrombocytosis
- Joint deformities: RA, Felty’s syndrome, SLE
- Lower extremity edema: Amyloidosis
g. Abnormal neurological examination:
- Essential thrombocytosis
- Non-Hodgkin’s lymphoma (NHL)
Differential diagnosis of splenomegaly:
- Enlarged left kidney
- Enlarged left lobe of liver
- Carcinoma of stomach
- Carcinoma of splenic flexure of colon
- Omental mass (TB or malignancy)
- Malignancy of tail of pancreas
- Ovarian tumor in females
C) Grading of Splenomegaly Based on Degree of Enlargement
1. Massive (>8cm or >5 fingers):
- Chronic Myeloid Leukemia (CML)
- Myelofibrosis
- Chronic Malaria, Chronic Kala-azar
- Gaucher’s disease
Tropical Splenomegaly Syndrome or Hyperactive Malarial Splenomegaly (HMS)
An idiopathic splenomegaly affecting malnourished children and adult ♀ in malaria-endemic regions eg. New Guinea, Africa, which may be a defective immune response to P malariae
- Clinical: Massive splenomegaly, asthenia, fatigue
- Lab: ↑ IgM antibodies against Plasmodium, ↓ T-helper cells ↓ CD4:CD8 ratio
2. Moderate (4-8cm or 2-4 fingers):
- Causes of massive splenomegaly
- Hemolytic anemia
- Portal hypertension
- Lymphoproliferative disorders: Lymphoma, CLL
3. Mild (<4cm or <2 fingers):
- Causes of moderate splenomegaly
- Infectious hepatitis
- Infectious mononucleosis (IM)
- Subacute Bacterial Endocarditis (SBE)
- Idiopathic Thrombocytopenic Purpura (ITP)
- Amyloidosis
- Sarcoidosis
- Felty’s syndrome
D) Lab Investigations:
1. Initial investigations:
- FBC with differential count
- Leucocytosis: Pyogenic infections, Leukemia
- Leucopenia: Malaria, Kala-azar, Enteric fever, Felty’s syndrome
- Pancytosis: Polycythemia
- Pancytopenia: Hypersplenism
- ESR
- Increased: Infection, SLE, lymphoma, severe anemia
- Decreased: Polycythemia
- Peripheral Blood Smear (PBS)
- Cell morphology: Leukemia, Hereditary spherocytosis, Thalassemia
- Parasites: Malaria, Kala-azar
- Reticulocyte count (Anemic patients)
- Increased: Hemolytic anemias
- Blood cultures (Febrile patients)
- SBE, Enteric fever
- Liver function tests
- Hyperbilirubinemia: Hemolytic anemias, Other hemolytic conditions, Hepatitis, Chronic liver disease
2. Additional investigations: Based on disease suspected by clinical and/or initial laboratory findings
- Hemoglobin electrophoresis (↑HbF in B-thalssemia)
- Coomb’s test (+ve in autoimmune hemolysis and -ve in hereditary spherocytosis)
- Red cell enzyme testing (G6PD deficiency)
- Osmotic fragility testing (+ve in Hereditary spherocytosis)
- Flow cytometry for lymphoproliferative profile (CLL, Hairy cell leukemia, lymphomas)
- Erythropoietin level (↓ in Polycythemia vera)
- Coagulation test (Chronic liver disease, DIC in AML, SLE)
- Serum lipase and amylase (Pancreatitis)
- Serum LDH (NHL, AML)
- Serum iron (↑ in Hemochromatosis, Thalassemia)
- Paul-Bunnell test (Infectious Mononucleosis)
- Congo red test (Amyloidosis)
- Serum ACE (Sarcoidosis)
- Napier’s Aldehyde test (Chronic Kala-azar)
- Anti-nuclear antibodies (SLE)
- Rheumatoid factor (RA, Felty’s syndrome)
- HBsAg (Hepatitis)
- Rose-Waaler test (Felty’s syndrome)
- Glucocerbrosidase activity (Gaucher’s disease)
- Sphingomyelinase (Niemann-Pick disease)
- Mantoux skin test (TB)
- Kveim skin test (Sarcoidosis)
3. Bone marrow aspiration and biopsy
- Myeloproliferative diseases
- Lymphomas
- Immunological diseases (Sarcoidosis, SLE, Felty’s syndrome, Amyloidosis)
- Gaucher’s disease
4. Lymph node biopsy
- Tuberculosis
- Sarcoidosis
- Lymphoma
5. Splenic biopsy
- Diagnosis of Lymphoma
- Niemann Pick’s disease (Large foamy cells)
- Amyloidosis (Large hyaline masses)
6. Liver biopsy
- Alcohol induced liver disease
- Hepatic steatosis
- Hemochromatosis),
7. Lung or Skin biopsy
- Sarcoidosis
E) Imaging:
1. To evaluate splenomegaly
- Ultrasonography
- CT scan
- Splenoportography
- Spleen liver colloid scan
- MRI
- Angiography
2. Confirming suspected diagnosis
- Chest X-ray:
- Miliary TB
- Lymphoma
- Sarcoidosis
- Extramedullary hematopoiesis in thalassemia
- Bone X-ray:
- Mosaic pattern in small bones of hand: Thalassemia
- Increased bone density: Myelofibrosis or Myelosclerosis
- Erlenmeyer flask sign in distal femur: Gaucher’s disease
- Skull X-ray:
- ‘Hair on end‘ appearance in Thalassemia
Investigations should be based on disease suspected by clinical and/or initial laboratory findings
SPLENECTOMY
1. Indications:
- Hodgkin’s lymphoma (for staging the extent of disease)
- Massive splenomegaly (for control of symptoms)
- Traumatic or Iatrogenic splenic rupture (for disease control)
- Hypersplenism or Immune-mediated destruction of one or more blood cell line (for correction of cytopenias)
Causes of Splenic rupture
- Trauma
- Infectious mononucleosis
- Leukemias
- Myelofibrosis
- Congestive splenomegaly
2. Problems after splenectomy:
- Immediate: Increased platelet count may lead to thromboembolic phenomenon
- Long-term: Increased risk of infection with capsulated organisms (like Streptococcus pneumoniae, Nisseria meningitidis, H.influenzae or E.coli), malarial parasites, babesia
Causes of Asplenism or Hyposplenism
- Asplenia: Dextrocardia
- Surgical: Splenectomy
- Diminished function: Sickle cell disease, Celiac disease, Dermatitis herpetiformis with enteropathy
3. Prophylaxis for Post-splenectomy infection:
- Vaccinate 2-3 weeks before elective splenectomy: Pneumococcal vaccine, Hemophilus influenza type B (Hib) vaccine, Meningococcal group C vaccine, Influenza vaccine
- Lifelong Antibiotic prophylaxis: Long-term penicillin V 500mg 12 hourly (erythromycin if allergic to penicillin)
- Revaccination of pneumococcal vaccine: in every 5 years and influenza vaccine anually
- Antimalarial chemoprophylaxis: if needed (travel to endemic area)
4. Post splenectomy hematological features:
- Thrombocytosis: persists in 30% cases
- WBC count: usually normal but there may be mild lymphocytosis and monocytosis
- Red cell morphology: Howell-Jolly bodies (Nuclear remnants), Pappenheimer bodies (contain sideroblastic granules), Heinz bodies (Denatured hemoglobin), Target cells, Nucleated erythrocyte (occasionally)
Sources:
- Harrison’s Principle of Medicine 16th Edition
- Davidson’s Principle and Practice of Medicine 20th Edition
- Bedside Clinics in Medicine Part I by Arup Kumar Kundu
- Kumar and Clarke’s Clinical Medicine 6th Edition
- Assessment of Splenomegaly – BMJ Best Practices