Definitions
Gait: Gait is the cyclical pattern of musculoskeletal motion that carries the body forwards. It involves a cyclic loss and regaining of balance by a shift of the line of gravity in relation to the center of gravity. Normal gait is smooth, symmetrical and ergonomically economical.
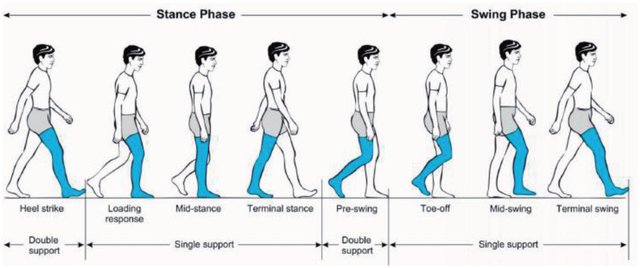
Gait cycle: The time interval or sequence of motions occurring between two consecutive initial contacts of the same foot, i.e., cycle of stance and swing by one foot.
Stance phase: When foot is on the ground and bearing weight (60% of gait cylce)
Swing phase: When foot is not bearing weight and moves forward (40% of gait cycle)
Double support phase: When both feet are on the ground simultaneously which occurs twice and comprises of 25% of normal gait cycle (absent in running)
Double float phase: When both feet are off the ground (present in running)
Step: The distance from one heel strike to next contralateral heel strike
- Normal: About 72 cm
Stride: The distance covered from one heel strike to the next ipsilateral heel strike (2 steps)
- Normal: About 144 cm
Cadence (step rate): Number of steps per unit time
- Normal: 90-120 steps/minute
Gait speed: Distance covered in a given amount of time
- Normal: 3 mph
Step or base width: The lateral distance between the heel centers of two consecutive foot contacts
- Normal: 5-10 cm or 2-4 inches)
Neuroanatomy of Gait
Walking requires the coordinated effort of several neurologic structures and functions:
- Frontal lobes: to generate the motor pathways to initiate gait
- Cerebellar and vestibular function: for co-ordination and balance
- Basal ganglia: for appropriate speed of movement
- Muscle strength: to move the legs and to overcome gravity to remain upright
- Sensation (particularly proprioception): to know where the feet and legs are in space
Normal Gait Cycle
1. Stance phase:
Mnemonic: I Like My Tea Pre-sweetened
1. Initial contact (heel strike)
2. Load response (foot flat)
3. Mid-stance (single leg stance)
4. Terminal stance (heel off)
5. Pre-swing (toe-off)
2. Swing phase:
Mnemonic: In My Teapot
1. Initial swing (acceleration)
2. Mid-swing
3. Terminal swing (deceleration)
Pelvic movement during gait
1. Lateral shift (pelvic list): Normally, pelvis and trunk shift 2.5-5 cm (1-2 inches) towards the stance phase leg to center the weight of the body
2. Vertical shift: Keeps the center of gravity from moving up and down more than 5 cm (2 inches) during normal gait
3. Pelvic rotation: Total of 8° pelvic rotation with 4° forward on the swing leg and 4° posteriorly on the stance leg
Muscle contractions
Concentric contractions of agonist muscle produce movement (when movement is against gravity)
- Quadriceps in load response/foot flat phase to produce knee extension against the gravity
Eccentric contractions of antagonist muscle control movement (when movement is towards gravity), e.g.
- Ankle dorsiflexors in load response/foot flat phase to control plantar flexion which occurs towards gravity
Isometric contractions stabilize the joint (when no movement occurs)
Top-down approach for gait analysis
1. Head and trunk position over the body
- Shoulders lift off on stance side to relieve pressure during antalgic gait
- Trunk sways towards affected side in trendelenburg gait
- Shoulder moves up and down on affected side in short-limbed gait
2. Hip
- Flex to 30 degrees and extend to 20 degrees in swing and stance phase during gait cycle
- Pelvis sags down on normal side in trendelenburg gait
3. Knee – does the patella face forward?
- Should have some flexion at initial contact
- Extends through stance phase
- Extend at toe off phase
4. Foot
- Foot progression angle (angle between the line from calcaneus to 2nd metatarsal and line of progression averaged from heel strike to toe off during stance phase of walking for each step)
- Angle of toe out (normally 8-15 degrees out-toeing)
- Push off
- Clearance in swing
Types or Patterns or Abnormalities of Gait
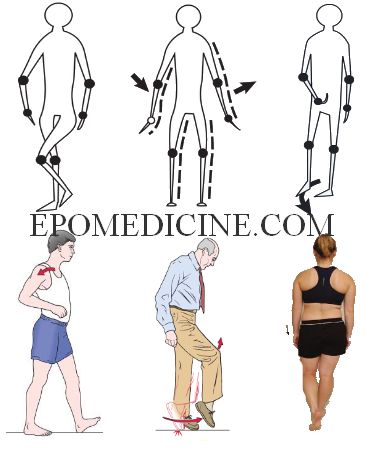
2nd row (from left to right): Gluteus maximus gait, Steppage gait, Trendelenburg gait
| Type of gait | Description | Probable diagnoses |
| Antalgic or painful gait | Patient does not bear weight on affected side and the body lurches to opposite side. There is decreased stance phase, stride length and step length. | Any painful lesion of the lower extremity i.e. foot, knee, hip |
| Toe-walking or Equinus gait | Heel strike is avoided | Heel pain Clubfoot Congenital short Achilles tendon Muscle spasticity (Cerebral palsy) |
| Quadriceps weakness gait | Inability to maintain knee extension at heel-strike and patient may push on thigh to extend the knee and lock | Quadriceps paralysis |
| Gluteus medius gait or Abductor lurch or Trendelenburg gait | Sound side hemipelvis drops downward during single-limb stance phase on weakened side (Trendelenburg gait) Lurch of body towards affected side in every stance phase (Abductor lurch; in contrast to the unaffected side in antalgic gait) | Polio Developmental Dysplasia of Hip Legg-Calve’s Perthe disease Slipped Capital Femoral Epiphysis Dislocated hip Fracture neck of femur Congenital coxa vara Gluteus medius paralysis |
| Gluteus maximus gait or Extensor lurch or Rocking horse gait | Trunk lurches backward at heel-strike on weakened side to interrupt forward motion of the trunk | Hip extensor weakness (e.g. poliomyelitis) |
| Flat foot or Calcaneal or Triceps gait | Absent push-off phase | Forefoot pain or rigidity Weakness of calf muscles |
| High stepping or Steppage or foot drop or Dorsiflexor gait | The affected foot is lifted high by flexing at hip and knee joint, in order to clear the toes from ground. The foot may audibly slap the ground and 1st strike is not with the heel. | Weak dorsiflexors Paralyzed dorsiflexors Common peroneal/fibular nerve palsy |
| Hip-hike gait | Hikes up the ipsilateral pelvis, in order to clear the floor | Stiff knee Foot drop |
| Circumduction gait | Lifts the entire leg higher than normal and swings the leg out along the side, in order to clear the floor (knee is extended and ankle is plantarflexed due to rigidity in UMN lesion) | Stiff hip gait Stiff knee gait Cerebral palsy Limb length discrepancy |
| Waddling gait | Bilateral drooping of hip (trendelenburg gait); Lurches on opposite side with wide base of support | Myopathies |
| Winking gait | Excess pelvic rotation in axial plane toward affected hip will demonstrate a pelvic wink. The pelvic wink produces extension and rotation through the lumbar spine to attain terminal hip extension. | Laxity Hip flexion contracture Anterior capsular injury or laxity |
| Ataxic gait | Wide-based gait (>2-4 inches); patient sways in different direction during ambulation | Cerebellar ataxia |
| Hemiplegic gait | Circumduction gait with affected arm, elbow and wrist flexed on the affected side | Hemiplegia |
| Paraplegic gait or Scissoring gait | Hypertonia in the legs, hips and pelvis means these areas become flexed to various degrees, giving the appearance of crouching, while tight adductors produce extreme adduction, presented by knees and thighs hitting, or sometimes even crossing, in a scissors-like movement while the opposing muscles, the abductors, become comparatively weak from lack of use | Spastic cerebral palsy (adductor contracture) |
| Stamping gait | Hard thump resulting from inability to perceive the distance between the foot and the floor | Posterior spinal column lesions |
| Short limb gait | <1.5 cm – compensated by pelvic tilt while walking Upto 5 cm – compensated by equinus >5 cm – patient’s body dips down on that side | |
| Shuffling or festinating gait | Short steps, stooped posture and patient is propelled forwards quickly as if trying to catch up with the center of the gravity which is placed anteriorly | Parkinson’s disease |
| Duck footed (slew-footed) gait | In-toeing | Increased femoral anteversion |
| Genu recurvatum gait | Hyperextension at knee | Paralysis of hamstrings (polio) ACL injury |
| Varus thrust gait | Varus (bow-leg) alignment as the limb accepts weight (stance phase), with a return to less varus and more neutral alignment during lift-off and the non-weightbearing (swing) phase of gait. | Posterolateral knee instability Pseudolaxity due to medial knee compartment osteoarthritis |
| Valgus thrust gait | Valgus (knock-knee) alignment visualized during the stance phase, with a return to less valgus (more neutral) alignment during lift-off and the swing phase of gai | Lateral comparment osteoarthritis |