Incidence the global incidence of neonatal sepsis at 5–6 per 1000 live births and that of meningitis at 0.7–1 (2.4–16 in South and South-East Asia, 6–21 in sub-Saharan Africa, and 1.8–12 in the Middle East and North Africa)1
Causative Agents :
- Group B streptococci
- Escherichia coli
- Klebsiella pneumoniae
- Streptococcus pneumoniae
- Listeria monocytogenes
- Enterobacter spp
- Citrobacter spp
- Pseudomonas spp and Serratia
- Staph aureus
- Coagulase negative Staphylococcus
Underlined = common
10 Diagnostic Dilemma in Neonatal Meningitis
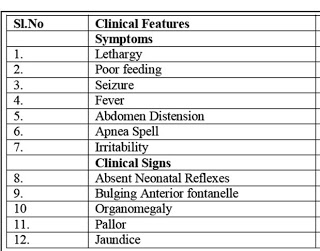
A. The well known “classical” symptoms often appear late in the course of the disease and their presence therefore predicts a worse outcome. Low level of consciousness at hospital admission which is known to be a predictor of poor outcome. Such features do not therefore allow the opportunity for early intervention.
B. Neonatal meningitis occurs in the absence of bacteremia and in the presence of normal CSF values. No single CSF value can be used to exclude meningitis, and peripheral WBC counts are also poor predictors of neonatal meningitis. The CSF culture is critical to the diagnosis, regardless of other laboratory results. PCR has high yield which is not always available in our setting.
C. It is important to bear in mind that a normal initial CSF white cell count, glucose and protein does not exclude bacterial meningitis. In a large series of 9,111 neonates who had an LP performed, 95 (1%) were found to have culture proven bacterial meningitis of whom 12/95 (13%) had normal CSF parameters It is also possible that a neonate with an initially negative CSF culture might develop evidence of meningitis in the context of ongoing bacteraemia.2 3
D. Defining Cerebrospinal Fluid White Blood Cell Count Reference Values in Neonates and Young Infants.
The 95th centile CSF WBC value for neonates without bacterial meningitis: 0–28 day old = 19 cells/cu.mm; 29–56 day old infants = 9 cells/cu.mm4
E. A traumatic tap:
6374 neonates had LP; 1.8% meningitis – 40% traumatic (>500 RBC/mm3)
CSF WCC adjusted “down” using several methods (500:1; FBC) did not improve diagnostic utility & decreased sensitivity.
If elevated CSF WCC manage as meningitis (PIDJ 2008;27:1047-51)
Abo et.al. used bedside ultrasonographic measurement of the interspinous space in various positions suitable. The position associated with the largest measurement in order:
- the sitting position with hip flexion
- the sitting position without hip flexion
- the lateral position with hip flexion and without neck flexion,
- the lateral position with both hip and neck flexion and finally,
- the lateral position without hip or neck flexion.
An important finding was that neck flexion did not increase the size of the interspinous space. Because neck flexion is associated with desaturation in the neonatal setting this provides further evidence that it should be avoided.5
F. Pretreatment with antibiotics does not prevent diagnosis
Those who received antibiotics 12 -72 h pre LP had significantly ↑ glucose and ↓ protein vs. those who did not receive them or received them < 4hr but there was no influence on CSF WBC. Hence, cases with high WBC treated as meningitis, has low likeliness to miss (Pediatrics 2008;122:726–730)
G. Does a Delay in the Laboratory Evaluation of the CSF Affect the Results?
Evidence suggests that a delay in laboratory analysis may affect the CSF results and even prevent an early diagnosis being made. Investigators compared CSF analysed immediately after it was obtained with the same samples of CSF analysed after a lag time of 2 h and 4 h. Where the baseline WCC was >30 cells/mm 3 , an early diagnosis of meningitis would have been missed in 53% if the samples at 2 h 79% if analysed at 4 h because of the decline in measured white cell count.6
H. Poor Prognostic Factors
- At 12 h after admission these were seizures, coma, use of inotropes, leucopenia < 5,000
- At 96 h after admission, seizure duration >72 h, coma, use of inotropes, leucopenia < 5,000.
- Abnormal EEG
These factors did not change when stratified according to causative pathogen.7
I. Role of Adjunctives
Dexamethasone – has no additional Benefit in Neonatal Meningitis mortality rates.
Oral glycerol- Glycerol quickly (within hours) increases plasma osmolality, which reduces excretion of CSF, and can improve brain oxygenation Glycerol has been studied in childhood meningitis but not explored in NNM Role is controversial even in childhood Meningitis
J. Tenth Question: Are we doing enough Lumbar puctures? Are we missing Neonatal Meningitis?
References:
1. Robillard P, Nabeth P, Hulsey T, et al. Neonatal bacterial septicemia in a tropical area. Four-year experience in Guadeloupe (French West Indies).Acta Paediatr 1993; 82:687–689. Stoll B.The global impact of neonatal infection. Clin Perinatol 1997; 24:1–21
2. Garges HP. Neonatal Meningitis: What Is the Correlation Among Cerebrospinal Fluid Cultures, Blood Cultures,and Cerebrospinal Fluid Parameters? Pediatrics. 2006;117:1094–100
3. Rajesh NT, Dutta S, Prasad R, Narang A. Effect of delay in analysis on neonatal cerebrospinal fluid parameters.Archives of Disease in Childhood – Fetal and Neonatal Edition. 2009;95:F25–F9
4. Kestenbaum LA, Ebberson J, Zorc JJ, Hodinka RL, Shah SS. Pediatrics. 2010;125:257–64.
5. Abo A, Chen L, Johnston P, Santucci K. Positioning for Lumbar Puncture in Children Evaluated by Bedside Ultrasound. Pediatrics. 2010;125:e1149–e53
6. Rajesh NT, Dutta S, Prasad R, Narang A. Effect of delay in analysis on neonatal cerebrospinal fluid parameters. Archives of Disease in Childhood – Fetal and Neonatal Edition. 2009;95:F25–F9.
7. Klinger G, Chin CN, Beyene J, Perlman M. Predicting the outcome of neonatal bacterial meningitis. Pediatrics.2000;106:477–82

MD Pediatrics and Fellowship Neonatology, he chooses to stay anonymous. He often writes his views online as well as share few important topics for medical students, doctors and specially parents. He does research in pediatrics.