Definition of Jugular venous Pulse and Pressure
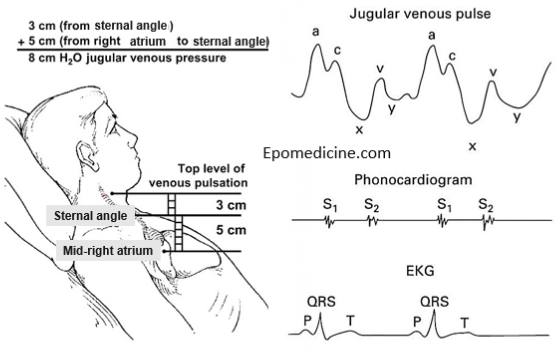
Jugular venous pulse is defined as the oscillating top of vertical column of blood in the right Internal Jugular Vein (IJV) that reflects the pressure changes in the right atrium in cardiac cycle. Jugular venous pressure (JVP) is the vertical height of oscillating column of blood.
Why is Internal Jugular Vein (IJV) preferred?
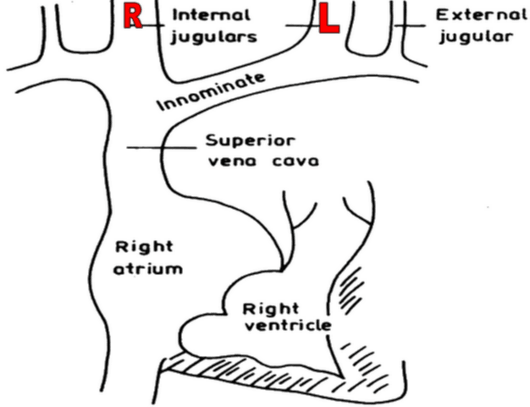
- IJV is anatomicallty closer to and has a direct course to right atrium while EJV does not directly drain into Superior venacava.
- It is valveless and pulsations can be seen. Due to presence of valves in External Jugular vein, pulsations cannot be seen.
- Vasoconstriction secondary to hypotension (as in COngestive heart failure) can make EJV small and barely visible.
- EJV is superficial and prone to kinking.
Why is Right Internal Jugular Vein (IJV) preferred?
- Right jugular veins extend in an almost straight line to superior venacava, thus favoring transmission of the hemodynamic changes from the right atrium.
- The left innominate vein is not in a straight line and may be kinked or compressed between Aortic Arch and sternum, by a dilated aorta, or by an aneurysm.
Evaluation of JVP
- Level
- Waveform
- Respiratory variation in level and wave pattern
- Hepatojugular reflux
- Venous hum
- Liver size and pulsations
Technique of measuring JVP
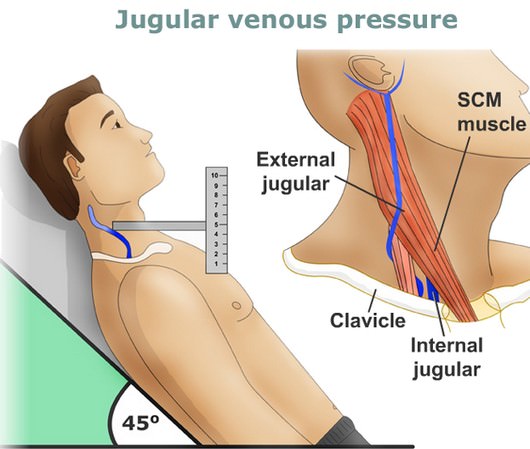
1) Position: Semi-reclining position with 45° angle between the trunk (not the neck) and the bed. Then, turn the head slightly towards left shoulder, so that the neck muscles are relaxed.
- Not in sitting position: because the upper level of venous column is below the clavicle
- Not in supine position: because the whole venous column moves beyond the angle of jaw into the intracranial cavity
2) Identify Jugular venous pulsation:
- Assure good lighting (can use tangential beam of light through torch).
- Look between the two heads of sternoclediomastoid.
- Note the upper level of pulsation, waveform and respiratory variation.
Do not mistake the carotid pulsations for venous pulsations.
| Jugular Vein | Carotid Artery |
|---|---|
| No pulsations palpable. | Palpable pulsations. |
| Pulsations obliterated by pressure above the clavicle. | Pulsations not obliterated by pressure above the clavicle. |
| Level of pulse wave decreased on inspiration; increased on expiration. | No effects of respiration on pulse. |
| Usually two pulsations per systole (x and y descents). | One pulsation per systole. |
| Prominent descents. | Descents not prominent. |
| Pulsations sometimes more prominent with abdominal pressure. | No effect of abdominal pressure on pulsations. |
3) Locate the sternal angle (Angle of louis):
- It can be felt as a transverse prominence, about 5 cm below the suprasternal notch at the level of 2nd costal cartilage.
4) Measurement:
- Measure the vertical distance (in cm) between the horizontal lines drawn from the upper level of venous pulsation and the sternal angle.
This can be done by using 2 rulers – one placed horizontal to the upper level of pulsation and another taking the vertical distance of that ruler from the sternal angle.
5) Calculate the right atrial pressure:
- Normally, the center of right atrium is 5 cm below the sternal angle. Hence, Add +5 cm to the above measurement to obtain the right atrial pressure.
6) Conversion:
- 1.3 cm of H2O or blood = 1 mmHg
Interpretation
1) Level:
Normal:
- From sternal angle: < 4 cm
- From center of right atrium: <9 cm
- In mmHg: <7 mmHg
Causes of elevated JVP (Jugular venous distension):
- Right ventricular failure
- Pericardial compression (constriction/tamponade) – little or no pulsations when severe
- Tricuspid stenosis
- Superior venacava (SVC) obstruction – no pulsations
- Circulatory overload
- Renal failure
- Excessive fluid administration
- Atrial septal defect with mitral valve disease
Causes of lowered JVP: Dehydration, Hypovolemia
2) Wave pattern:
The normal JVP consists of 3 ascents or positive waves (a,c and v) and 2 descents or negative waves (x,x’ and y):
- a wave (ascent): due to active atrial contraction leading to retrograde blood flow into neck veins
- x wave (descent): Due to continued atrial relaxation
- c wave: due to impact of the carotid artery adjacent to the jugular vein and retrograde transmission of a positive wave in the right atrium produced by the right ventricular systole and the bulging of the tricuspid valve into the right atrium.
- x’ wave (descent): due to descent of floor of right atrium (tricuspid valve) during right ventricular systole and continued atrial relaxation
- v wave (ascent): due to passive atrial filling (venous filling)
- y wave (descent): due to opening of tricupsid valve and subsequent rapid inflow of blood from right atrium into the right ventricle leading to a sudden fall in right atrial pressure.
The best way to identify the waves (ascents and descents) would be to simultaneously auscultate and observe the wave pattern.
- ‘a’ ascent: clinically corresponds to S1 (though it actually occurs before S1); sharper and more prominent than ‘v’ wave
- ‘x’ descent: follows S1; less prominent than ‘y’ descent
- ‘c’ ascent: occurs simultaneously with carotid pulse; but never seen normally
- ‘v’ ascent: coincides with S2; less prominent than ‘a’ ascent
- ‘y’ descent: follows S2; more prominent than ‘x’ ascent
Note: h wave – between the bottom of ‘y’ descent and beginning of ‘a’ ascent, during the period of diastasis (relatively slow ventricular filling).
Mnemonic: Function at waveform points – ASK ME
- Atrial filling
- Systol
- Klosed tricuspid
- Maximal atrial filling
- Emptying of atrium
Abnormalities of JVP
- Prominent ‘a’ waves (Giant a-wave or Venous corrigan): due to resistance to atrial emptying at –
- Tricuspid level: tricuspid stenosis, right atrial tumors
- Right ventricular level: concentric hypertrophy due to severe pulmonary hypertension, right ventricular cardiomyopathy, severe aortic stenosis, acute pulmonary embolism, acute tricuspid regurgitation
- Cannon waves: Very prominent ‘a’ waves due to atrial contraction against closed tricuspid valve
- Regular cannon waves: Junctional rhythm, Ventricular tachycardia 1:1 retrograde conduction, Isorhythmic AV dissociation
- Irregular cannon waves: Complete heart block, Ventricular tachycardia, Ventricular ectopy, Ventricular pacing, Classic AV dissociation
- Absent ‘a’ waves: Atrial fibrillation (AF), Post DC conversion of AF, Sinoventricular conduction in hyperkalemia
- Single wave:
- ‘a’ and ‘v’ wave merge: Heart rate > 120/min
- early ‘v’ wave with obliterated ‘x’ wave: Severe chronic tricuspid regurgitation, acute tricuspid regurgitation
- Absent ‘x’ wave (failure of atrial pressure to fall): Atrial fibrillation, Severe chronic tricuspid regurgitation, Acute tricuspid regurgitation, Constrictive pericarditits
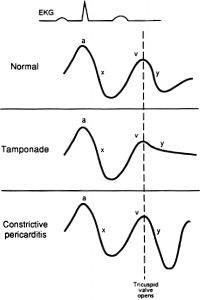
- Prominent ‘x’ wave: Cardiac tamponade
- Prominent ‘v’ wave: Right ventricular failure, Tricuspid regurgitation, Atrial septal defect with or without mitral regurgitation
- Diminished ‘v’ wave: Hypovolemia, venodilators
- Rapid ‘y’ descent: Causes of prominent ‘v’ wave, constrictive pericarditis (Friedrich’s sign)
- Slow ‘y’ descent: Tricuspid stenosis, Percardial tamponade, Tension pneumothorax
3) Venous hum: Continuous bruit over neck veins (normally noiseless) due to increased velocity of blood flow or decreased viscosity of blood.
Causes:
- Physiological: Children, Pregnancy
- Pathological: Hyperkinetic states, Anemia, Thyrotoxicosis, Beriberi, Intracranial AV fistula
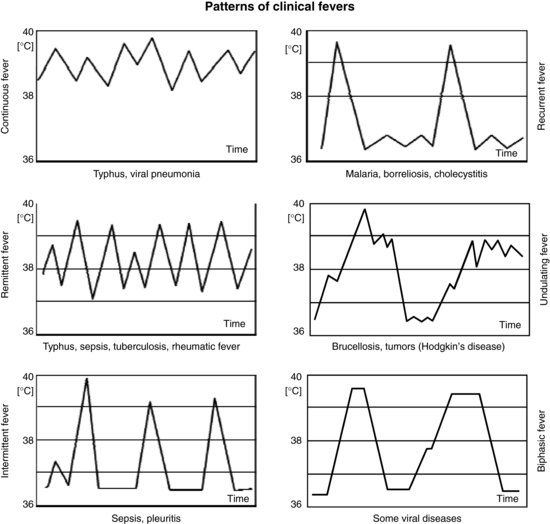
4) Respiratory variation:
Normal: Venous column rises during expiration and falls during inspiration
Reason: During inspiration venous return to the right side of the heart increases due to increased negative thoracic pressure. However, this is accommodated by the inspiratory decrease in pulmonary vascular resistance. As a result, pulmonary artery, right ventricle and right atrial pressures fall inspite of increased venous return. During expiration, due to increased positive intrathoracic pressure, pulmonary circulation is compressed by the thoracic cage resulting in increased pulmonary resistance and pressure.
Kussmaul’s sign: Paradoxical rise in JVP during inspiration
Causes: Constrictive pericarditis, Cardiac tamponade, Restrictive cardiomyopathy
Reason: Increased venous return in inspiration cannot be accommodated as increased pulmonary filling leading to inspiratory filling of neck veins
5) Hepatojugular reflux (Provocative test):
Technique: When pressure is applied over the liver by pressing firmly below the right costal cartilage margin f0r 30 seconds, the venous pressure gets exaggerated initially due to increased venous return. Later the myocardium accomodates the extra venous return and the level falls.
Positive test: Rise in JVP for >10 seconds
-
- Early cardiac failure
- False positive: Valsalva (abdominal guarding), fluid overload
False negative: SVC/IVC obstruction, Budd chiari syndrome
This test also helps to differentiate venous pulsation from the arterial pulsation.
6) Liver pulsations:
In an infant, the liver is the only guide to the recognition of elevated right atrial pressure as the JVP is difficult to delineate.
- ‘a’ wave: clinically appears after S1
- ‘v’ wave: clincally appears fater S2
Summary:
| JVP Clues | Interpretation |
| Level of JVP | Level of right atrial pressure, right ventricular filling pressure, Central venous pressure |
| Elevated pulseless JVP | SVC obstruction |
| y descent | Pattern of right ventricular filling or right atrial emptying |
| Rapid y descent | Rapid filling (Right ventricular failure, Tricuspid regurgitation, Constrictive pericarditis) |
| Slow y descent | Slow filling (Tricuspid stenosis) |
| Obliterated y descent | Little or no filling (tamponade) |
| Prominent a wave | Resistance to pre-systolic right atrial emptying (Tricuspid stenosis, non-compliant right ventricle) |
| Venous hum | Hyperkinetic circulatory state (Anemia, thyrotoxicosis) |
| Analysis of rhythm | Sequence of atrioventricular contraction (AV dissociation, Complete heart block, Junctional rhythm) |
JVP in Constrictive pericarditis and Cardiac tamponade
Mnemonic: PaY TaX (Remember: X descent is prominent in both)
Pericarditis (constrictive) – Y descent is prominent
Tamponade – X descent is prominent (Y descent is lost)
Pericardial pressure is distributed equally among all chambers since pericardial fluid is free flowing. This reduces the gradients between chambers throughout diastole. This is inconsequential in small effusions, but becomes hemodynamically significant in large effusions in which a greater pressure in the pericardium is transmitted to all four cardiac chambers resulting in “equalization of central pressures”. The reduction of the pressure gradient between the atria and the ventricles when the AV valves open mean that there is less transfer of blood from the atria to the ventricles. This is seen as a loss of the y-descent of the CVP or PCWP waveform tracings.
– In contrast, the thickened pericardium in constrictive pericarditis does not restrict chamber enlargement at low volumes and therefore does not impair early diastolic filling but at higher volumes the limiting constraint is reached and filling is limited and the pressures in all chambers will become equal. Filling is preserved in early diastole but compromised in late diastole.
Very nicely presented..a great job indeed
very good
Should the image say sternal angle not sternal notch?
Great observation. Thank you. The picture shall be corrected and changed.
I have like the presentation help me to get more prevention on your website please
Very nicely explained.Excellent for medical students and fresh residents.
Very nice
Very well tackled… Very well explained to understand. Thanks.
Well presented… Information is helpful during clinicals..
this was very helpful for me to find answers for my pg preparation mcqs. thank you very much
great job, thank for your article
Excellent
nice explanation
Simple and practical . great . thanks
Thanks a lot!
This article is really helpful and reliable.
Thank you very much .. crisp understanding ☺️
excuse me ,how is jvp waveform recorded ?
do we observe for example a or v wave or is there a device to record these waves?
because i think it is hard to notice canon a wave or other changes in jvp waveform from observation