A Single Male baby was born at 38 weeks of gestation with birth weight of 3.1 kg through Normal vaginal delivery. At birth the child had cried immediately. At 15 minutes of life, the child developed central cyanosis. There was no respiratory distress and heart rate was normal range.
Child was shifted immediately to NICU. Saturation was 70% and which reached upto 84% with oxygen supplementation. On auscultation, chest was unremarkable but on cardiac auscultation, a faint murmur could be heard. Hyperoxia test was also performed and the baby failed the hyperoxia test.
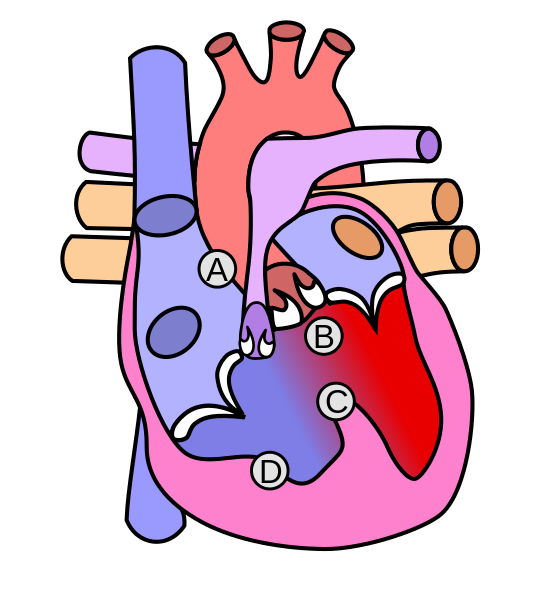
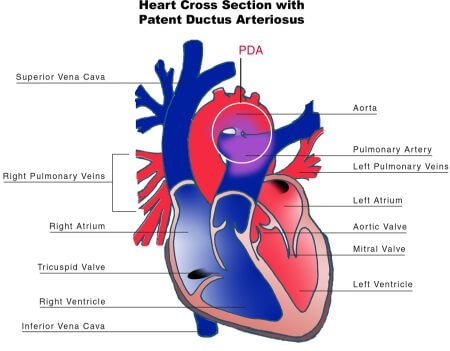
Immediately echocardiographic screening was done to look for possible presence of a duct dependent circulation. Echocardiography showed large VSD (Ventricular septal defect) with over-riding of Aorta with severe pulmonary stenosis. PDA was seen with left to right shunt measuring 3mm. It was case of TOF (Tetralogy of Fallot) with PDA (Patent Ductus Arteriosus) – a ductus dependent circulation as the baby had severe PS (Pulmonary Stenosis).
Chest Xray showed oligemic lung fields with upturned apex of the cardiac silhouette.
In any scenario, Prostin (PGE1) would have been started but since echocardiography showed patent PDA, it was withheld and monitoring was planned. On the second day, the baby was deteriorating, saturation was not maintained and reached as low as 60%. In general, SpO2 above 75% is adequate for Cyanotic heart diseases. Echocardiography was reassessed and the PDA was still patent at 2-3mm. The desaturation was not explained by CHD. So, the child was kept under CPAP and finally intubated for the drop in saturation.
After intubation, the SpO2 worsened to 30-40%. Since the cardiologist was at the spot, reassessment was done with Echocardiography. PDA was patent with 2 mm size. A trial of PGE1 (Prostin) was given. After 5 minutes, SpO2 improved to 60%, heart rate improved from 100 to 120 and by 10 minutes SpO2 was 87% under MV and the baby looked much better.
Retrospective analysis:
It was a case of a closure or narrowing of PDA in a duct dependent circulation. The child was saved by PGE1 which keeps the PDA open, until the definitive management – BTS (Blalock Taussig Shunt).
A PDA connects the proximal left pulmonary artery to the descending aorta just distal to the left subclavian artery and is important in the foetal circulation as it diverts blood flow from the right ventricle to the descending aorta.

MD Pediatrics and Fellowship Neonatology, he chooses to stay anonymous. He often writes his views online as well as share few important topics for medical students, doctors and specially parents. He does research in pediatrics.