A 31 weeks of gestation baby was born through emergency LSCS for Severe maternal hypertension. At birth baby required resuscitation and baby was intubated and transferred to NICU for ventilation. Fluids and Inotropes were started and ABG was sent. Vitamin K was given stat. Blood gas showed severe metabolic acidosis, therefore calculated amount of bicarbonate correction was done in slow infusion. Routine investigations were sent and IV antibiotics were started. Ventilator settings were optimized. Repeat blood gas showed correction in metabolic and respiratory status.
His Complete blood count showed Thrombocytopenia with platelets of 30,000/cumm. Rest investigations were within normal limits. Hemoglobin was 19g/dl. Baby had good urine output and stable vitals on support.
On Day 2, baby had prominent pallor and tachycardia. There was no obvious GI bleeding and no bleeding in the Endotracheal tube. Abdomen was normal. On further examination, anterior frontanelle was tense and pupils were unequal.
A presumed diagnosis of Intraventricular Hemorrhage was made. Hemogram and hematocrit was repeated and blood products were ordered. Fluid bolus was given and inotrope was escalated. Vitamin K was repeated. PT and aPTT was slightly prolonged. Hemoglobin had dropped to 12g/dl. Pack RBC was transfused.
What were the risk factors for Intraventricular bleed?
- Maternal hypertension: there have been reports of severe maternal hypertension leading to fetal IVH.
- Prematurity: < 32 weekers are at increased risk of IVH
- Very Low Birth weight: Weight < 1.5 kg was another risk factor
- Asphyxia at birth: At birth the baby was limp and required resuscitation. CNS ischemia, reperfusion injury could be another risk for IVH.
- Mechanical ventilation: Adds on to risk of IVH in preterm, especially if baby has to struggle on ventilators.
- Others: Hyperosmolar medicines, fluid bolues which were unavoidable part of management.
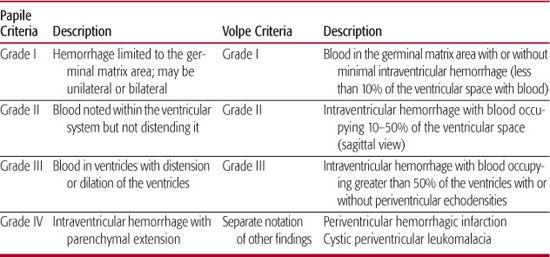
On day 3, baby had persistent drop in hematocrit. Head size was increased with separation of sutures. Sunset sign was seen. A request for portable Cranial USG was made and USG confirmed our diagnosis. USG revealed Grade III Intraventricular hemorrhage (Volpe’s grading ). Grade III IVH has a grave prognosis seen as neurological morbidity and mortality. It was a Catastropic diagnosis and a case of Catastropic IVH.
In a one and half year, this was probably the first case of severe IVH in our setting. I had seen plenty of cases of grade I and II IVH in preterm neonates during my fellowship training, most of which required follow up USG scan and carried a good prognosis. Also few cases of severe IVH requiring Shunt surgery were also encountered. As one of my seniors always said, “If a baby has severe BPD and Severe IVH – it’s the worst diagnosis for all – baby, doctor and parents”. Even in cases of severe BPD, the child fails to thrive and are left neurologically and chronically disabled with episodes of severe BPD spells requiring hospital care.
Suggested Reading for IVH in Neonates
https://www.ucsfbenioffchildrens.org/pdf/manuals/49_IntraventricularHem.pdf
https://www.slhd.nsw.gov.au/rpa/neonatal/html/docs/ivh.pdf

MD Pediatrics and Fellowship Neonatology, he chooses to stay anonymous. He often writes his views online as well as share few important topics for medical students, doctors and specially parents. He does research in pediatrics.