Definition of Low Back Pain
Low back pain (LBP) is defined as pain, muscle tension or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain (sciatica). “Diagnostic triage” after excluding non-spinal causes of low back pain classifies LBP into 3 broad categories:
- Specific spinal pathology (<1%)
- Radicular syndrome (5-10%)
- Non-specific low back pain (90-95%; diagnosis of exclusion)
Non-specific low back pain is subclassified according to the duration:
- Acute: <6 weeks
- Subacute: 6-12 weeks
- Chronic: >12 weeks
- Recurrent: period of LBP lasting more than 24 h preceded and separated by a period of at least 1 month without LBP (de Vet definition)
Origin of Back Pain
| Mechanical | Non-mechanical | Visceral |
| Soft tissue (Lumbar strain/sprain) | Neoplasm | Pelvic organ disease |
| Muscle/fascia (Myofascial pain) | Infection | Renal disease |
| Discs (Herniated discs, Discogenic pain) | Inflammatory | Abdominal aortic aneurysm |
| Joints (Facet joints, Sacroiliac joint) | Metabolic | Gastrointestinal disease |
| Bone (Vertebral fractures, Spondylolisthesis, Kyphosis, Scoliosis) |
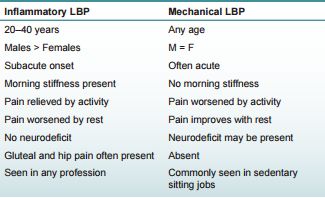
Nature of Back Pain
Mechanical vs Inflammatory Back Pain:
ASAS criteria for inflammatory back pain will be discussed later.
Back pain with leg pain:
Back pain with leg pain must be classified as either referred or radicular pain whenever possible.
| Referred pain | Radicular pain |
| Back > Limb | Limb > Back |
| Dull ache | Lancinating |
| Above knee | Below knee (usually; S1 occasionally felt in thigh & buttock only) |
| Unilateral or Bilateral | Unilateral |
| Non-dermatomal | Dermatomal |
| No aspect (front/back/side) or edge | Aspect and edge |
| No sensory symptoms | +/- sensory symptoms (inflamed root = pain; non-inflamed root = paresthesia) |
| No neurological signs | +/- neurological signs |
| Straight leg raise (SLR) – ?back pain worse | SLR – leg pain worse |
Vascular claudication vs Neurogenic claudication:
| Vascular Claudication | Neurogenic Claudication |
| Triggered by increased demand across arterial stenosis. Relieved by rest. | Triggered by lumbar extension worsening spinal stenosis. Relieved by lumbar flexion. |
| Pain reliably comes after a fixed amount of exertion (e.g. specific walking distance) | Pain may come with minimal exertion (e.g. standing in line, going down stairs) |
| Pain comes with activity even if back is flexed (e.g. riding a bicycle) | Pain does not occur with exertion in lumbar flexion (e.g. riding a bicycle or walking uphill) |
| Cramping pain – distal to proximal | Numbness, aching – proximal to distal |
Natural History of Low Back Pain
- At least 50% of these people will recover within 2 weeks and 90% within 6 weeks, but recurrences are frequent.
- After 6 weeks, improvement is slowed.
- Cumulative risk of at-least 1 recurrence within a 12 month period is 73%.
- Only 5% of people with an acute episode of low back pain develop chronic low back pain and related disability.
Flags in Back Pain
- Red flags: Indicate potential serious pathology
- Yellow flags: Risk factors for chronicity, the psychosocial barriers to recovery
- Orange flags: Psychiatric issues in patients with back pain
- Blue flags: Occupational issues
- Black flags: Organizational barriers to recovery
5 Goals of Low Back Pain Assessment
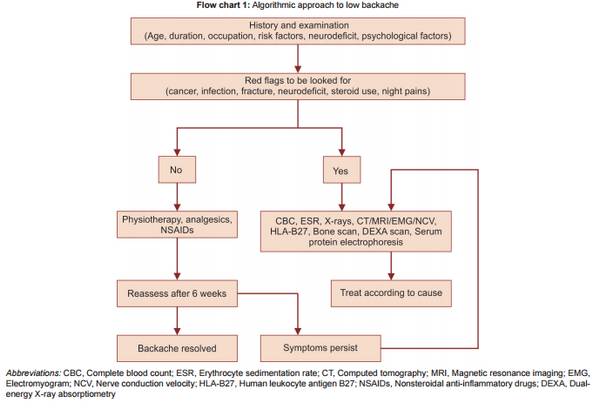
There are 5 main goals of low back pain assessment and are listed sequentially below:
- Ruling out potentially serious spinal pathology (Red flag signs)
- Ruling out specific causes of Low Back Pain
- Ruling out substantial neurologic involvement
- Evaluating the severity of symptoms and functional limitations
- Identifying the risk factors for chronicity (Yellow flag signs)
Red Flag Signs in Low Back Pain
Red flag signs are the indicators of serious spinal pathology and suggests for additional investigations or urgent evaluation.
Mnemonic: TUNIC
Red flag signs are used to rule out following causes of low back pain and the questions and examinations must be directed to rule them out:
1. Trauma (Spinal fracture)
2. Unresponsiveness to therapy >1 month
3. Neoplasm (Spinal cancer)
4. Infection (Spinal infections)
5. Cauda equina syndrome
Additional red flags for children:
- Age <4 years
- Pain that interferes with daily activity
- Limp or altered gait
- Back pain despite no clear mechanism of injury
- Acute or repetitive trauma
| Disorder | Symptoms | Signs |
|---|---|---|
| All | Duration of pain > 1 month Bed rest with no relief | |
| Cancer | Age ≥ 50 years History of cancer Unexplained weight loss | Neurologic findings Lymphadenopathy |
| Compression fracture | Age ≥ 50 years (> 70 years is more specific) Significant trauma History of osteoporosis Corticosteroid use Substance abuse | |
| Infection | Fever or chills Recent skin or urinary tract infection or catherterization Immunosuppression Injection drug use | Fever (temperature > 100°F or 38°C) Tenderness over spinous processes |
| Cauda equina syndrome | Saddle anesthesia Bilateral sciatica or leg weakness Difficulty urinating Fecal incontinence | Progressive motor or sensory deficit |
Ruling out Specific Causes of Low Back Pain
Classic discogenic history (factors that worsen pain):
- Sitting > Standing > Lying
- Arising from seated position
- First 20-30 minutes of day
- Coughing, sneezing, straining (Valsalva maneuver)
- Lifting weight out in front of the body
- Twisting
- Bending at waist
Differentials of back pain according to age groups:
- Children: Scoliosis, Spondylolisthesis, Infections, Calve’s disease
- Adolescents: Scheuermann’s disease, Scoliosis, Mechanical back pain, Spondylolysis, Infections, Adolescent intervertebral disc disease
- Young adults: Mechanical back pain, PIVD, Spondylolisthesis, Spinal fracture, Ankylosing spondylitis, Coccydynia, Infections, Spinal stenosis
- Middle aged: Mechanical back pain, PIVD, Scheuermann’s disease and old fracture, Spondylolisthesis, Rheumatoid arthritis, Spinal stenosis, Paget’s disease, Coccydynia, Spinal metastases, Pyogenic osteitis of spine
- Elderly: Osteoarthritis, True senile kyphosis, Osteoporosis +/- fracture, Osteomalacia +/- fracture, Spinal metastases
| Disease | Features | Relation to movement/position and Response to treatment |
| Annular tear | Age – 4th decade Non-radicular axial back pain Discogenic history | Improved with passive extension, side gliding, proper body mechanics |
| Paramedian protrusions & herniations | Age ~40 yrs Back + Leg pain (In variable percent) Discogenic history Radiculopathy: 90-95% involve L5-S1 (S1 may present as calf cramps) Recurrences – common Positive dural tension signs | Pain increases with ipsilateral weight bearing on sitting/standing Comfortable in lateral decubitus or supine with hips and knees flexed Larger herniations – uncomfortable in standing and extension Pain centralizes with extension or side gliding Pain peripheralizes with flexion activities or manipulation |
| Lateral & foraminal herniations | Age ~60 yrs Leg pain > Back pain May not have discogenic history L4-L5 (60%); L3-L4 (30%); L5-S1 (<10%) Recurrences – uncommon Positive dural tension signs | Pain is worst with standing or walking erect Often uncomfortable in bed; many sleep sitting Sitting usually relieves pain Generally more resistant to mobilization, centralization and traction |
| Upper lumbar protrusions and herniations (above L4) | Age ~55 years Risk: prior L4-S1 fusions L1-L2, L2-L3: groin, anterior thigh, back pain L3-L4: extension to knee, medial leg Positive dural tension sings | |
| Sequestered disc herniations and disc fragments | Discomfort during Valsalva maneuver or lifting abruptly resolves Back pain decreases and lower extremity pain increases | |
| Cauda equina syndrome | Risks: Tumors (50%), Central L3-L4, L4-L5 discs Bladder incontinence Bowel incontinence Sexual dysfunction Diminished perineal sensation Bilateral lower extremity neurologic complaints or pain | |
| Lumbar stenosis | Age >55 years Spontaneous, insidious onset with gradual progression Central stenosis – bilateral symptoms, fairly symmetrical but non-specific distribution Lateral or Foraminal stenosis – unilateral symptoms, fairly specific dermatomal distribution | Increased symptom on extension Symptoms: walking (neurogenic claudication) > standing > lying Sitting – often asymptomatic Valsalva – doesn’t affect pure stenosis Flexion relieves symptoms (going uphill, bicycling, shopping cart sign) Flexion exercises may provide transient relief only; Chairs and corsets that place patient in flexion may provide relief |
| Spondylolisthesis – Isthmic | Age – Late childhood/Adolescence Risk: Athletes (sports with significant lumbar extension & rotation – gymnastics, dance, martial arts, crew) L5-S1 involvement Intervertebral slip by inspection or palpation | Worsened with extension Segmental hypermobility by use of manual passive physiological intervertebral motion test |
| Spondylolisthesis – Degenerative | F>M; Old age L4-L5 involvement Unilateral radicular symptom (due to foraminal stenosis) Intervertebral slip by inspection or palpation | Worsened with extension Segmental hypermobility by use of manual passive physiological intervertebral motion test |
| Tumors | Age – 20 (Benign tumors); 50 (Malignancy) Constant pain awakening the patient or persists beyond 1 month despite treatment Smoking history B symptoms, Dry cough, Change in bowel/bladder habit Benign – Osteoid osteoma and Osteoblastoma (pain relived by aspirin) Malignant primary tumor – Multiple myeloma Metastatic tumors (bronchogenic, breast, prostatic, renal) – 2 patterns of pain (mild local complaints progressing to severe radiculopathy OR sudden pain due to pathological fracture or instability) | Unrelated to position |
| Herpes Zoster radiculopathy | History of cancer Spontaneous onset Pain may precede vesicular lesion by upto 3 weeks and usually lasts through eruption period 10-20% have post-herpetic pain (common in older patients) Single, unilateral dermatome involved (thoracic root in 50%) – initially dysesthesia, full paresis occurs within hours to days (55% recover fully) | No relation with position, movement or activities |
| Diabetic radiculopathy | Middle-aged or Elderly Pain – constant and worse at night Sensory and Motor complaints common | |
| Arachnoiditis | Risks: Disc space infections, Subarachnoid hemorrhage, Multiple surgeries, Intrathecal drugs, Radiation therapy, Myelography Reproduction of lumbar or lower extremity symptoms with long stride or cervical and thoracic flexion No discogenic history | |
| Sciatic neuropathy | Blunt/penetrating injuries or Traction injuries (hip surgery) or Tumors or Compression (Wallet sciatica, Piriformis syndrome) Neurologic complaints and deficits are more common than pain No discogenic history | No relation to spinal posture or Valsalva maneuver |
| Piriformis syndrome | Double devil (Trigger point pain + Sciatic nerve entrapment) Trigger point pain – Back pain, buttock pain, posterior thigh pain Sciatic nerve entrapment – Paresthesias &/or numbness in calf and foot Externally rotated attitude of affected leg Reproduction of symptoms: 1. Freiburg’s sign – Forceful internal rotation of flexed hip 2. Bonet’s sign: Add adduction (i.e. FAIR test) 3. Pace maneuver: Resisted abduction and external rotation of hip in sitting position Piriformis tenderness (Along the line drawn from greater trochanter to sacroiliac end of greater sciatic foramen in lateral position with affected limb up and hip flexed to 90 degrees) | |
| Facet joint pathology (Facet syndrome) | Conditions associated – Osteoarthritis, Instability, Acute subluxation Onset relates to increased axial loading and hyperextension activities Axial back pain No localizing neurologic signs | Pain with extension and ipsilateral side bending and rotation Pain: Standing > Sitting Dramatic response to facet manipulation and facet joint injection |
| Strains | Uncommon but over-diagnosed Pain with stretch or prolonged contraction of involved muscle | |
| Sacroiliac joint pain | Risks: Mid-pregnancy to postpartum period, Seronegative spondyloarthropathy, After trauma, After extensive spinal fusion Gradual or sudden onset Pain in sacroiliac region or buttock (usually unilateral); may cause posterior thigh or groin pain 3 positive out of 5: Distraction, Compression, Thigh thurst, Ganselen’s test, Sacral thurst | Patient feels best when reclining Pain with vasalva maneuver may be present |
| Spinal fractures | Traumatic or Osteoporotic (postmenopausal and prolonged corticosteroid use) Commonly involves T10-L1 May result in leg pain and occasionally neurologic symptoms | Increased pain with changing positions Generally worse in spinal flexion |
| Ankylosing spondylitis | Younger male (AS, Reiter’s) Lower lumbosacral pain Morning stiffness (“gel”) of 2-3 hours (20-30 minutes in disc disease) Positive modified Schober’s test Reduced chest expansion Enthesopathy (heel pain) Radiographic sacroilitis Elevated ESR or HLA-B27 | Pain improved with activity |
| Spinal infections | Risks: Immunosupressed patients, Prior sepsis, Prior spinal procedures Constant pain awakening the patient Radiculopathy, fever and constitutional symptoms may be present Epidural abscess – progresses quickly Vertebral osteomyelitis – average delay to diagnosis is 3 months (TB has more slower course) | Pain doesn’t relate well to position or movement |
| Vascular claudication | History of smoking, diabetes or hyperlipidemia Sudden or gradual onset Asymmetrical involvement of calves Leriche syndrome – buttock claudication and impotence due to aorto-iliac occulsive disease | Increased work demands on lower extremity musculature worsen symptoms Walking uphill increases symptoms Claudication symptoms caused by cycling and walking are relieved by cessation of activity Standing, sitting or flexion do not reproducibly relieve symptoms |
| Abdominal aortic aneurysm | Medical background same as for vascular claudication Pain – Lumbar, constant, gradually worsens | Unrelated to motion |
| Viscerogenic | Prostatitis, Renal disease, Stomach and duodenal diseases, Pancreatic diseases, Retroperitoneal disease, Gynecologic disorders Pain modified by state of activity of viscera | Unrelated to position or motion |
| Nonorganic or Psychogenic | Malingering – Intentional Depression, Anxiety, Hysteria – Unintentional See the Wadell signs below (DoREST mnemonic) |
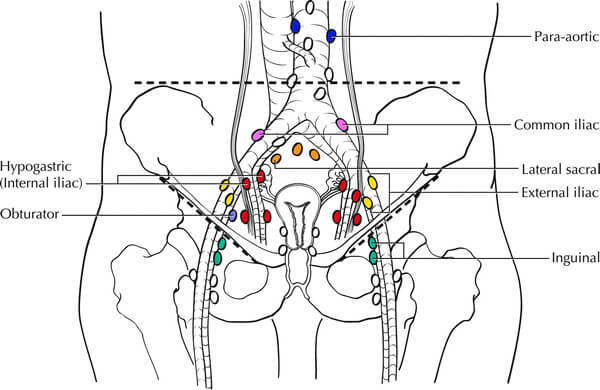
Diagnosis of Pseudospine pain
| Condition | Diagnostic keys |
| Abdominal aortic aneurysm | Age >50 years Abdominal and back pain Pulsatile abdominal mass Curvilinear aortic calcification in X-rays |
| Endometriosis | Women of reproductive age Cyclic back and pelvic pain |
| Pelvic inflammatory disease | Young, sexually active woman Systemically ill (fever, chills) Discharge, Dysuria |
| Ectopic pregnancy | Missed period Abdominal and/or pelvic pain Positive pregnancy test |
| Prostatitis | Men >30 years Dysuria Low back and perineal pain Tender, boggy prostate gland |
| Nephrolithiasis | Flank and groin pain Hematuria Costovertebral angle tenderness |
| Pancreatitis | Abdominal pain radiating to back Systemic signs Elevated serum amylase |
| Perforated duodenal ulcer | Abdominal pain radiating to back Air under diaphragm on erect Chest X-ray |
| Fibromyalgia | Young to middle-aged woman Widespread pain Multiple tender points Disrupted sleep, fatigue Normal radiographs and lab values |
| Polymyalgia rheumatica | Age over 50-60 years Hip or shoulder girdle pain and stiffness Elevated ESR Dramatic response to low dose prednisone |
| Seronegative spondyloarthropathies | Younger male (AS, Reiter’s) Lower lumbosacral pain Morning stiffness (“gel”) Improvement with activity Positive modified Schober’s test Reduced chest expansion Enthesopathy (heel pain) Radiographic sacroilitis Elevated ESR or HLA-B27 |
| Forrestier’s disease (DISH) | Age >50-60 years Thoracolumbar stiffness > pain Flowing anterior vertebral calcification over 4 contiguous vertebrae No sacroiliac invovlement Normal ESR and CRP |
| Piriformis syndrome | Buttock and leg pain Pain on resisted hip external rotation and abduction Transgluteal or transrectal tenderness 3 or more wedged vertebrae with endplate irregularities |
| Trochanteric bursitis, gluteal fasciitis | Gluteal and leg pain Pain lying on affected side or with crossed-leg Pain or tenderness over greater trochanter frequently with iliotibial band tightness and tenderness |
| Osteoporosis | Woman >60 years Severe pain (fractures) Aching dull thoracic pain relieved in supine position (mechanical) Loss of height, increased thoracic kyphosis |
| Osteomalacia | Diffuse skeletal pain or tenderness Increased ALP |
| Paget’s disease | Bone pain: low back, pelvic, tibia Nerve root entrapment (hearing loss, spinal stenosis) Increased ALP “Picture frame” vertebra in X-rays |
| Proximal motor neuropathy | >50 years Diffuse leg pain, worse at night Proximal muscle weakness |
| Malignancy | >50 years Back pain unrelieved by position change – night pain Previous history of malignancy Elevated ESR |
Evaluating the Severity of Symptoms and Functional Limitations
There are numerous rating scales and scoring systems to assess the severity of low back pain. A simple assessment tool developed by Higuchi et.al. may be useful at bedside.
a. Pain intensity: 3 parameters scored on scale of 0 (no pain) to 10 (worst pain) and average of 3 is calculated
- Current pain
- Average pain during last 6 months
- Worst pain during last 6 months
b. Pain interference:
- Almost daily back pain during past 6 months: 1 point
- Affect on work activity:
- Sick leave: 2 points
- Other: 1 point
- Non-work activity affected: 1 point
- Treatment during last 6 months:
- Alternative medicine: 1 point
- Physician: 1 point
- Both: 2 points
Interpretation:
- Mild: Pain interference <3, Pain intensity <5
- Moderate: Pain interference <3, Pain intensity >/= 5
- Severe: Pain interference >/= 3
Source: Higuchi, Y., Izumi, H., & Kumashiro, M. (2010). Development of a simple measurement scale to evaluate the severity of non-specific low back pain for industrial ergonomics. Ergonomics, 53(6), 801–811. doi:10.1080/00140139.2010.489652
Yellow Flag Signs in Low Back Pain
These are psychosocial factors shown to be indicative of long term chronicity and disability.
Mnemonic: ABCDEFS
Attitude: Negative
Behavior: Fair avoidance
Compensation issues
Depression and anxiety
Expectation: Passive treatment better than active (expectation that pain will increase with work and activity)
Financial problems
Social issues: History of sexual abuse, physical abuse, lack of support, older age, overprotective family
- A negative attitude that back pain is harmful or potentially severely disabling
- Fear avoidance behavior and reduced activity levels
- An expectation that passive, rather than active, treatment will be beneficial
- A tendency to depression, low morale, and social withdrawl
- Social or financial problems
Inflammatory Back Pain and Axial Spondyloarthritis
Inflammatory back pain mnemonic (Positive if 4 out of 5): ERIN40
- Exercise – improvement
- Rest – no improvement
- Insidious onset and persisting for >3 months
- Night pain
- <40 yrs age at onset
European Spondyloarthropathy Study Group (ESSG) Criteria
Inflammatory spinal pain OR Synovitis and 1 of the following: AS DIP
- Alternating buttock pain
- Sacroiliitis
- Diarrhea, cervicitis or urethritis occurring within 1 month before the onsent of arthritis
- Inflammatory bowel disease
- Psoriasis
- Positive family history
ASAS classification for axial spondyloarthritis: SPINEACHE mnemonic
1. Sacroilitis on imaging (by radiograph or MRI) + >/= 1 of SPINEACHE OR
HLA-B27 + >/= 2 of SPINEACHE
2. SPINEACHE
a. Sausage digit (dactylitis)
b. Psoriasis-positive family history of SpA
c. Inflammatory back pain
d. NSAID good response
e. Enthesitis (heel)
f. Arthritis
g. Chron’s colitis/disease – elevated CRP
h. HLA-B27
i. Eye (Uveitis)
New York Criteria for Ankylosing Spondylitis
Bilateral sacroiliitis grade 2 or higher OR Unilateral sacroiliitis grade 3 or higher and 1 of the following:
- Inflammatory back pain
- Limitation of lumbar movements in sagittal and frontal planes
- Decreased chest expansion (1 inch or less at 4th ICS)
ACR Criteria for Diagnosis of Fibromyalgia
Mnemonic: WOKE UP STIFF (this also reminds that non-restorative sleep and morning stiffness are also important features of this disorder although not included in the criteria)
- Widespread pain AND 11 out of 18 tender points (9 pairs)
- Tender points (9 pairs):
- Occiput: suboccipital muscle insertion
- Knee: medial fat pad
- Epicondyle: 2 cm distal to lateral epicondyles
- Upper outer quadrant of buttocks
- Parasternal: second costochondral junction
- Supraspinatus muscles: at origins, above scapula spine
- Trapezius muscles: upper border, midpoint
- Intertransverse spaces at C5-C7, anterior aspects
- Femoral greater trochanter: posterior to prominence
- Four kg: approximate force on digital palpation
History Taking For Low Back Pain
In general, a history must obtain following informations:
- Acute/Subacute/Chronic/Recurrent back pain
- Axial/Radicular/Referred pain
- SOCRATES of pain (Inflammatory vs Mechanical; Discogenic/Stenosis/Non-spinal, etc.)
- ADL (Activities of daily living) affected (Severity of Symptoms)
- Red flag signs
- Yellow flag signs in cases of subacute and chronic back pain
- Screening question for depression in chronic back pain: Ask 2 questions (highly sensitive but not specific)
- Have you often been bothered by feeling down, depressed or helpless?
- Have you often had little interest or pleasure in doing things?
- If ‘yes’ response for both the 2 questions above: Is this something you would like help with? (increases specificity)
- Patient’s occupation, demands, ICE history (Ideas, Concerns and Expectations)
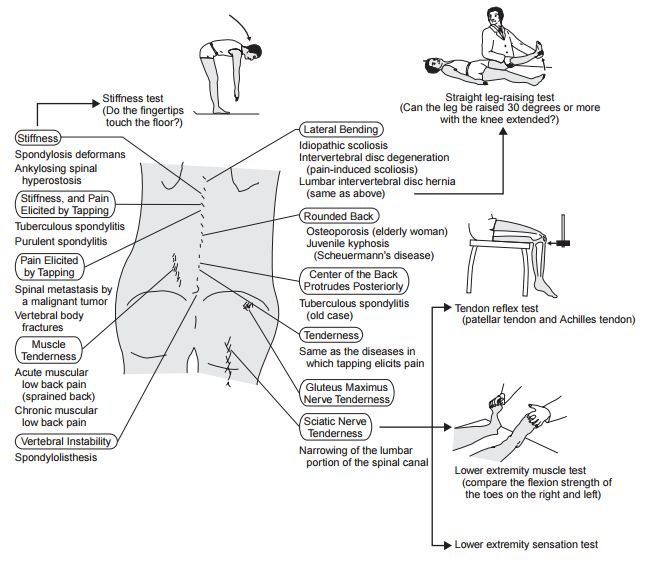
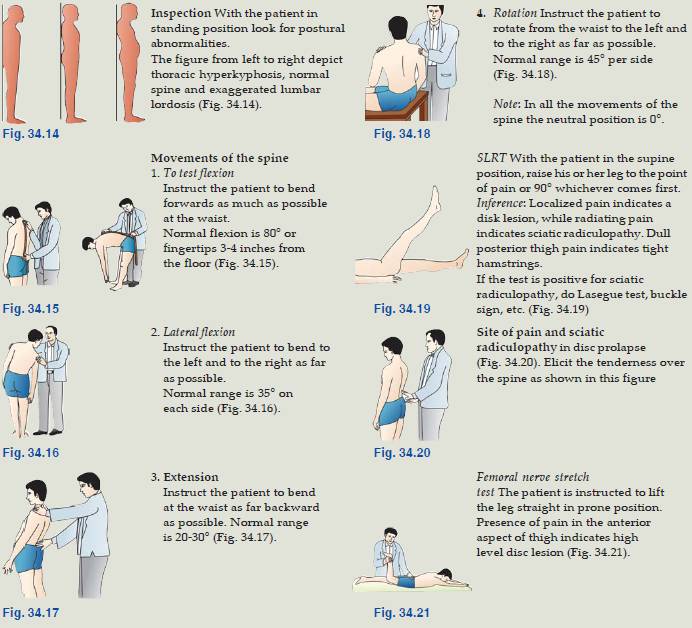
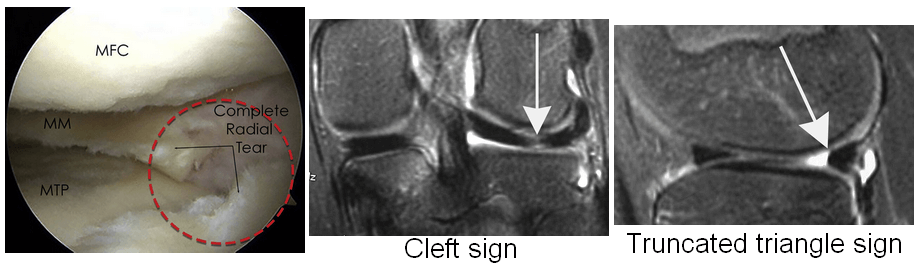
Physical Examination in Low Back Pain
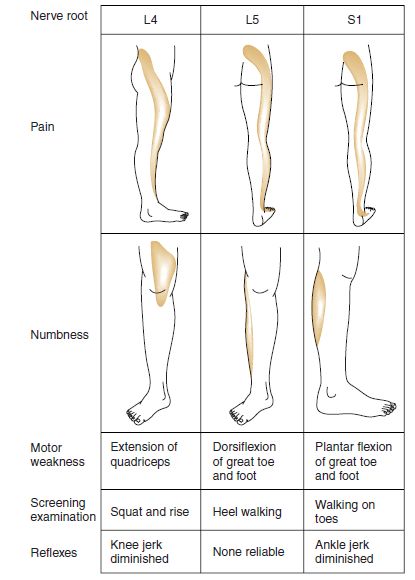
- Radiculitis = lower limb pain and neurological signs
- Nerve root sleeve involvement = neurological signs (conduction block), radicular pain (radiculitis), back pain (inflammation of dura)
List – deviation to opposite side: shoulder type PIVD
List – deviation to same side: axillary type PIVD
Braggard’s test involves dorsiflexing the foot after lowering the hip flexion by 10-15 degrees from point of SLR positive. Neri’s test involves flexing the neck. SLR detects tension on nerve root L4, L5, S1. Reverse SLRT or Femoral nerve stretch test detects tension in the L2–L4 nerve roots. With the patient prone, pain elicited in the anterior thigh with extension of the hip or flexion of the knee confirms a positive RSLR test.
Wadell’s sign (Non-organic cause of Back Pain)
Wadell’s sign indicate psychological distress (nonorganic causes of pain): 3 out of 5 is significant
Explore these signs in cases of non-specific back pain.
Mnemonic: DOReST
- Distraction testing: Inconsistent responses noted with the same test when performed in a standard fashion and when the patient’s attention is distracted (eg. flip test – seated straight leg raising without discomfort versus radiating pain with supine straight leg raise)
- Overreaction: Disproportionate verbalization, facial expression, muscle tension, tremor, collapsing, and even profuse sweating (single most important sign but observer dependent)
- Regional disturbances: in strength and sensation that do not correspond with nerve root innervation patterns
- Stimulation testing: Pain on simulated axial loading by pressing on the top of the head or simulated spine rotation
- Tenderness: Localized tenderness that is does not follow a dermatomal or expected referral pattern; superficial light touch over the low back causing severe discomfort, or deep palpation causing widespread discomfort through the thoracic spine or sacrum or hips
Apply 4 tests:
- Skin roll test: gently roll loose skin of lower back
- Twist test: gently rotate patient’s torso at hips
- Head compression test: apply small load to top of head
- Flip test: test straight leg raise when seated and supine
Summary:
References:
- da C Menezes Costa L, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. 2012 Aug 7;184(11):E613-24. doi: 10.1503/cmaj.111271. Epub 2012 May 14. PMID: 22586331; PMCID: PMC3414626.
- https://musculoskeletalkey.com/physical-examination-in-radiculopathy/
- Low Back Pain – Handbook
- Evidence based management of Low back pain

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.
Ok
Nice Information
Hmm thanks for sharing this information with us, i hope every one getting good experience from this article.
its superb presentation
can’t believe
very vast
great work
Thank you for this article, I am currently using it to study for my NP Finals. It is very thorough and comprehensive.
Thank you for the great explanation!
Could you tell us the source of each photograph you used from a book or site?
Thank you in advace!