Most patients have only one operation in their lives and to them, it is of great concern and a Solemn Occasion, though it is just another Appendix/Hernia/TKR to the Surgeon.
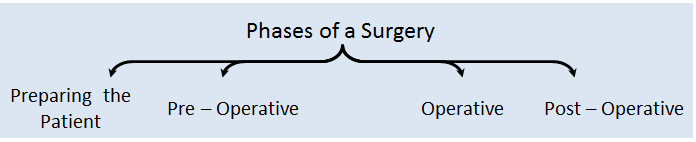
Being a part of a surgical team is where one shares their knowledge, experience and responsibility with the others. This should be in terms of patient care, methods of surgery and management of complications. Responsibilities of the members of the team may be divided into phases.
On presenting to the Clinic / Out-Patient Department (OPD)
Duty of a Surgeon does not begin from the Operating Room (OR) but the Out-Patient Department (OPD) / Clinic.
On presentation of a patient to the Clinic, one has to note the complete history, conduct a thorough review of systems and a physical examination apart from the area of concern of the patient. Following a systematic questionnaire and examination will prevent one not to miss any essential information from the patient.
Once relevant information and condition of the patient are gathered and a provisional diagnosis is framed, a battery of laboratory investigations is ordered to support the provisional diagnosis and uncover any unknown and hidden pathology which may cause complications during or after surgery.
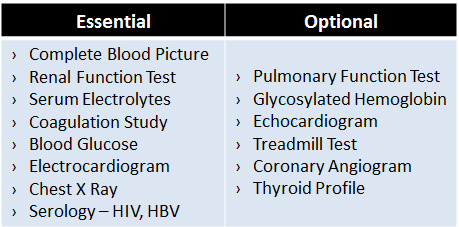
Table 1. Most common laboratory investigations performed for fitness.
A risk assessment is then conducted whether the patient is deemed fit for surgery or has to be managed by medications. Here a consultation of a physician or anaesthetist can be taken.
Once the patient is considered fit for surgery, s/he is then counselled regarding further procedures.
If the patient is not regarded as fit for surgery, other modalities of treatment have to be explored which do not pose much threat to an already diseased body.
An exception to the above procedure is during Emergency, where Surgery needs to be performed to save the life even in a person associated with co-morbidities the duration of this phase has to be cut short. In such a situation a combined effort of surgeon, anaesthetist and physician has to be contributed to the care of the patient during and after surgery.
Preparation of the Patient
This is the phase where the patient and doctor’s interaction needs to be taken with utmost care and sympathy. It should be given adequate time to make sure the patient and the relatives are convinced about the situation. The choice has to be given to the patient for further treatment after explaining all the advantages and disadvantages of all the available modalities of treatment.
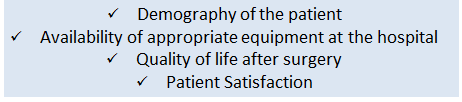
The choices of the treatment have to be decided to consider the following parameters:
Once the decision has been made by the patient and relatives, a consent form has to be signed by the patient him/herself if the patient is above the consenting age or is physically and mentally capable of giving consent, else the consent needs to be taken from the responsible caretaker (content of the consent form has to be explained orally also) and all their questions are to be cleared. They must always be explained about the need to revert to alternate surgical options in case the planned surgery cannot be instituted due to various factors. Possibilities of recurrence (if any) must be clearly explained.
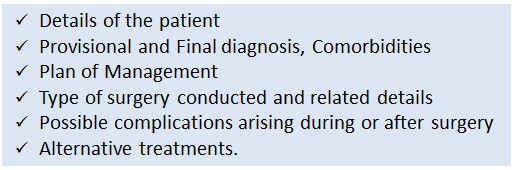
Box 1. Essential points which have to be included in a Consent Form.
A list of all the medications used by the patient has to be procured. Non-essential and potentially dangerous drugs need to be stopped (Eg. Anti-Coagulants). Essential medications and the ones which have a significant risk of rebound phenomenon on stopping the drug may be continued (Eg. Bronchodilators). The ones which have been stopped should be resumed as and when it is feasible.
Behavioural modification may also be prescribed to the patient such as to stop smoking, exercise and preoperative respiratory muscle training. These are quitting to smoke to reduce the operative & postoperative complications and hospital stay.
An Anaesthetist has to be consulted to obtain a fitness for surgery and their orders have to be added to the advice the surgeon gives to the patient.
The patient is then given a date for elective surgery and is advised to come back a day before to the Hospital, provided the patient follows all the precautions and orders given by the surgeon and anaesthetist.
An exception to the above procedure is during Emergency, where Surgery needs to be performed to save the life even in a person associated with co-morbidities the duration of this phase has to be cut short and quick action has to be taken. In such a situation a combined effort of surgeon, anaesthetist and physician has to be contributed to the care of the patient during and after surgery.
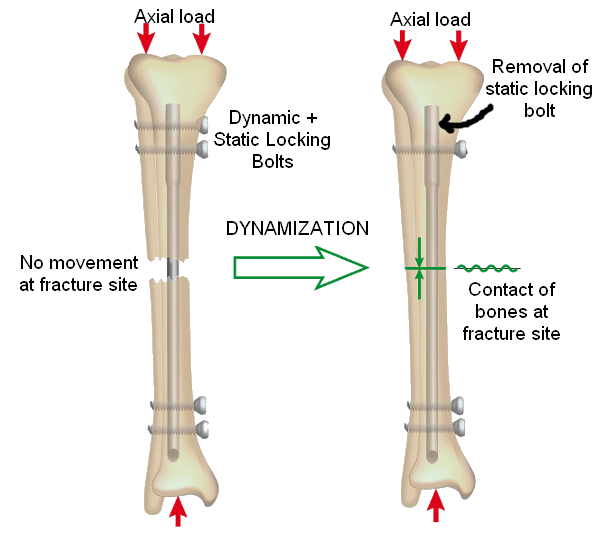
Damage Control Surgery
In a severely injured patient, Damage Control Surgery (Abbreviated Laparotomy) is conducted where physiological recovery is preferred over anatomical recovery i.e., minimal intervention is preferred initially only to bring the physiology back to normal. In such a situation the phase of preparation of patient should be cut short but essential work should not be ignored such as Consent, Medications taken etc.
The intention to consider physiological recovery is to cure the lethal triad of Injury which may lead to mortality of the patient if ignored.
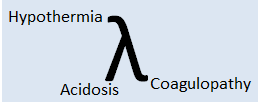
Fig 1. Lethal Triad of Injury
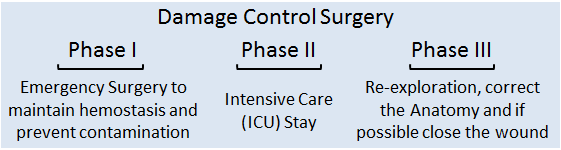
Box 2. Phases of Damage Control Surgery
Pre – Operative Management
This phase includes all the procedures which are done after the admission of the patient into the hospital. Here the details of the patient, diagnosis and the procedure to be conducted are verified and the “Informed Consent” if not taken has to be made sure it is done.
If needed a Physician and Anaesthetist review may be done if the patient is with comorbidities.
Medications and Procedures
Antimicrobial Agents have to be prescribed to prevent Wound Infections –
1. Inj. Ceftriaxone 1gm / Cefuroxime 1.5 gm (against Gram-Negative Bacteria), generally administered just before surgery.
2. Inj. Metronidazole 500mg (against Anaerobic Bacteria, during GIT Surgeries)
Analgesics –
1. Inj. Voveran i.e., Diclofenac Sodium 75mg (acts as an antipyretic too)
2. Inj. Buscopan i.e., Hyoscine 10mg (smooth muscle relaxant & antiemetic)
Antiemetics – Inj. Ondansetron 4mg (antiemetic).
Other Pre-Operative Medications –
1. Inj. Ranitidine 150mg / Inj. Pantoprazole 40mg (raise pH)
2. Inj. Metoclopramide 10mg (reduce gastric secretions and increase the tone of LES)
3. Inj. Tetanus Toxoid 0.5ml
4. Tab. Diazepam (reduces anxiety)
Patient may require Thromboembolism prophylaxis following risk assessment on individual basis.
It is ensured that any medications recommended by the anaesthetist or physician are given to the patient.
Secure an Intravenous cannula, Foley’s Caterer (based on the procedure conducted other essential equipment are made sure are in place).
Administration of Intravenous fluids, mainly crystalloids.
A major surgery which expects major blood loss, the blood of the patient is to be cross-matched. The blood bank has to be informed about the surgery and reserve is made sure is available for use.
All the related investigations are to be made sure they are present and updated. Imaging modalities which are needed during surgery have to be checked and kept safe.
Instructions to the Patient
The patient should be Nil per Oral from the night before (in Emergency, Ryle’s tube to be placed and contents should be emptied).
Surgical area to be cleaned with antibacterial agent and hair to be clipped. An antiseptic shower may be prescribed the night before surgery.
Bladder and Rectum have to be emptied.
As the patient is being prepared for the surgery, it is equally important for the surgeon to prepare for the planned surgery.
Operative Phase
The most essential phase of a Surgeon is in the Operating Room. The anatomy and the procedure have to be refreshed the day before the surgery.
The patient is carefully shifted from the room/ward to the Pre-Operative Room. All the requirements for surgery (drugs, suture, staples, drains, catheters and prosthesis) and anaesthesia (anaesthetic drugs, ET Tube, catheters, Needles) have to be prepared well in advance to prevent unnecessary delay during the surgery.
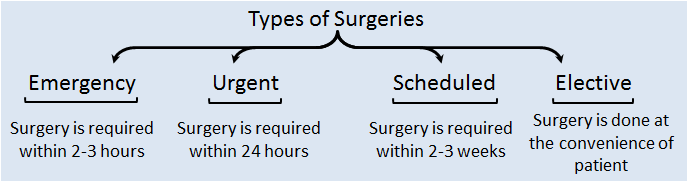
Box 2. Classification of Surgeries based on the time between presentation and operation.
Order of patients posted to surgery: Emergency → Urgent → Scheduled → Elective.
Sign In
SIGN IN – Once the patient is placed on the Operation Table, his/her name, diagnosis, surgery to be performed, surgical site are read out loud and noted. Also, consent is checked if taken or not.
The anaesthetist takes over and provides the appropriate anaesthesia (General, Epidural, Spinal or Regional) based on the type of surgery planned. If it is a minor surgery, local anaesthesia is administered after draping the patient.
The Surgeon, Assistant Surgeon and Assisting Nurse Scrub up (a thorough hand wash with antiseptic solution from fingers to elbow and rinse in the hand – up, elbow – down position and eith the same position maintained surgical gown is put on and gloves are donned).
Time Out
TIME OUT – The patient is now under anaesthesia, now the patient details are once again confirmed, the procedure is crosschecked, the surgical site is confirmed, all the team members introduce themselves, antibiotic prophylaxis is given, sterility of instruments is confirmed and essential images (X-Ray / CT / MRI) are displayed.
Surgical Site is identified and prepared with antiseptic solution twice with separate swabs (Eg. For limb surgeries – one joint above and below, abdomen surgeries – from nipples to mid of thigh).
The patient is then draped with sterile cloths with a window towel over the surgical site.
An appropriate blade is chosen depending on the length of the incision. The incision is made in a single stroke with smooth movement and consistent depth and speed. Constant traction is provided perpendicular to the direction of the incision to prevent sawing of the margins. Diathermy may also be used to make an incision by using the cutting mode at the skin and coagulation mode at the deeper layers.
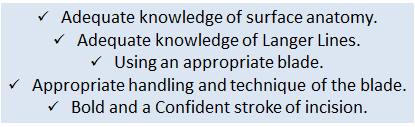
Box 3. Principles of making an incision.
The procedure of the planned surgery is executed, provided hemostasis is maintained. It is made sure that the time taken to wrap up the surgery is as short as possible to prevent Post-Operative Surgical Site Infections.
Closure of the wound depends on the initial character. Closing a clean wound would not be an issue, whereas for a contaminated wound a delayed closure is recommended to reduce risk of infection.
A Drain may be placed to prevent collections in the anatomical cavities.
The abdomen is wiped off of any blood stains and the wound is cleaned with a bactericidal solution and an Antiseptic Bandage is applied.
Sign Out
SIGN OUT – After closing the wound, before leaving the Operating Room, the surgeon confirms the procedure planned and procedure conducted and a note of it is made, the count of swabs and instruments are verified, any specimen collected is sealed and labelled with the details of the patient and outcome of the surgery with the postoperative management is recorded (record includes recommendations of the surgeon and anaesthetist).
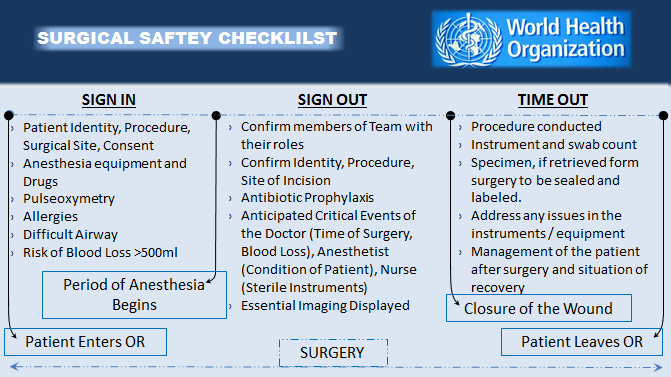
Box 4. Scheme of WHO Patient Safety Checklist – Surgical.
Post – Operative Period
As soon as the Operating Room is evacuated and the patient is brought to the Recovery Room, the operative procedure has to be recorded in the case file of the patient, which includes the detailed steps of the surgery, any medications used intra-operatively and the amount of blood loss and the further medications and management.
The Surgery is technically over, but the patient is the Surgeons responsibility till s/he leaves the hospital.
Immediate postoperative care is the most essential, where the patient is to be monitored until consciousness is regained (in case of General Anesthesia). During this period the surgeon is responsible for the surgical site and the anaesthetist for the remaining. Once the patient stabilizes s/he can be shifted to the Post-Operative Room.
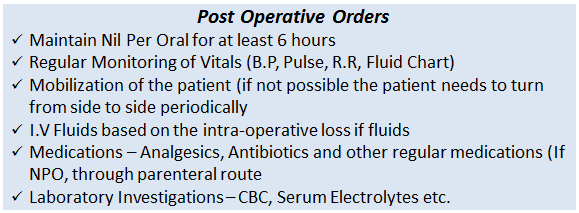
Box 5. Most Common Post-Operative Orders.
There may be changes in the orders based on the type of surgery conducted.
S.O.A.P
There needs to be timely monitoring of the patient in a structured manner, to prevent missing any events in the post-operative time.
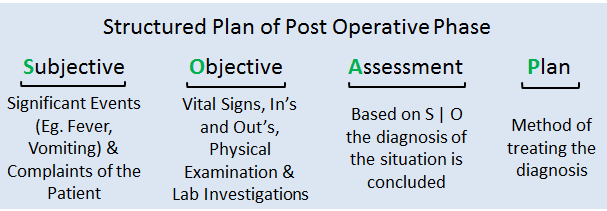
Box 6. S.O.A.P format for Post-Operative Phase.
S – Every checkup after the surgery has to begin with any Events which have occurred from the last checkup. Such as Fever, Wound Bleed, Wound Ooze, Sleep, Vomiting or Drop on blood sugar level. Complaints of the patient have to be noted. Such as Pain or difficulty in tolerating food.
O – Vital Signs have to be monitored regularly (Blood Pressure, Pulse, SpO2 and Respiratory Rate). A cardiac patient may be checked with Central Venous Pressure and Electrocardiogram. Fluid balance has to be noted i.e., intake and output of fluids by the patient. The amount of collection in surgical drain must be noted. The Surgical Area needs to be inspected to identify any issues with the wound (drain if placed has to be checked). Essential laboratory investigations might be ordered to know the status of the physiology (Complete Blood Picture, Serum Electrolytes, Blood Sugar etc.)
A – The above findings have to be summarized to conclude as to what the problem is.
P – The problem which has surfaced from the assessment has to now be solved. Such as Fever – Antipyretics, Vomiting – Antiemetics, Pain – Slight increase in the dose of Analgesics, Wound Ooze – Identify the type of secretion and act accordingly (Increasing Antibiotic Spectrum, Redressing the wound).
Apart from this, there has to be a regular change of the dressing/bandage of the wound to prevent further accentuation of Surgical Site Infection.
The most widely accepted standard for discontinuation of drain is a volume 30 mL/day for 24 hours.
Depending on the status of healing of the wound, sutures may be removed according to the area of the body.
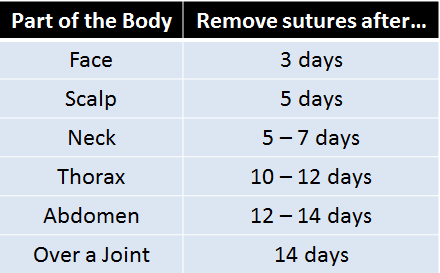
Table 2. Duration after which sutures have to be removed based on the part of the body
Discharge
Discharge of the patient depends on recovering from the surgery (duration is based on the type). At this time the patient and the relatives need to be explained regarding the type of surgery conducted, precautions needed to be taken, food restrictions and time to rejoin work and clear all their queries.
The patient needs to be explained the importance of rehabilitation and its effect in improving the quality of life post-surgery. All the medications which were used before surgery can be resumed added with the present ones (antibiotics, analgesics etc.). Complications of the surgery have to be explained and the respective symptoms have to be informed to them (to reach the hospital as early as possible if any arises).

Table 3. Complications of conducting a Surgery
As clearly depicted in the above table, Postoperative complication seems to be more in number and severe, hence it is said: “Success of one’s Surgery depends on the Post-Operative Care taken.”
Summary
Surgery is one of the departments where most of the patients get better which is recognized by the patient and the relatives themselves and are satisfied, which makes the surgeons even more careful, sympathetic towards them. Also, knowledge and skills are the ones which are essential to treat the patient.
It is generally said –
“A good surgeon knows how to operate,
A better surgeon knows when to operate
And the best surgeon knows when not to operate.”
Process of taking a patient into surgery is divided into four phases – Preparing the patient, preoperative period, operative phase and postoperative period. Every phase is important and should not be neglected.
Before deciding about the surgery being conducted, the patient and relatives are given the choice regarding the option of surgery or not. If they prefer surgery all the modalities available are put forward with the advantages and disadvantages.
Once the procedure is finalized the patient is admitted into the hospital and the necessary approvals from the physician and anaesthetist are taken and the patient is adequately prepared for the day of surgery.
The day of surgery is the essential phase where the patient is gotten rid of his presenting complaints. The time of surgery is to be kept as short as possible to minimize the risk of Surgical Site Infections.
The postoperative period is also where the patient is to be given the utmost care, many of the complications which occur can be prevented by timely monitoring, examination, assessment and responding appropriately.
The patient is discharged based the recovery s/he shows, this should be accompanied by advising the patient and relatives the importance of rehabilitation, medications and regular clinic visits. They also have to be informed about the potential complications and their respective symptoms.

Graduated from one of the famous institutions in Telangana, Kamineni Institute of Medical Sciences. He has always been fond of writing articles in Medicine. Since the undergraduate years was interested in making creative Presentations and taking seminars.


Nice collection there. I will definitely share with my friends. Any time specification for starting preoperative antibiotics before the start of surgery?
Thank You Dr. Venkat in showing interest in the content and sharing with your friends.
Sir, This is a topic where previously it was recommended to administer the antibiotics during the time of anesthesia, but in the recent times studies have shown better outcome (i.e. less risk of SSI) if they were given within 60 minutes before making the incision.
Whereas, WHO suggests prophylaxis can be given within 120 minutes without risk and they say there has been no significant difference between administering within 120-60 minutes vs. within 60 minutes.
Also the dose has to be repeated if duration of the Surgery exceeds 2 Half-Lives of the drug or when there is a major blood loss.
Nevertheless, Antibiotic Prophylaxis has to be continued till 24 hours post surgery.
You may visit these for more information:
1. https://www.ashp.org/-/media/assets/policy-guidelines/docs/therapeutic-guidelines/therapeutic-guidelines-antimicrobial-prophylaxis-surgery.ashx
2. https://www.who.int/gpsc/Appendix5.pdf?ua=1
3. https://www.who.int/gpsc/appendix25.pdf?ua=1