Introduction
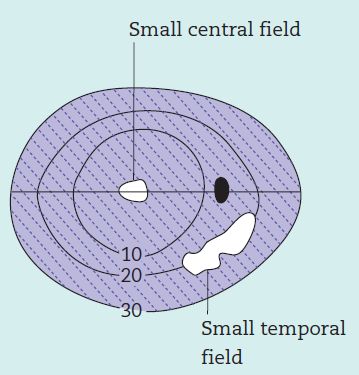
Field of vision or Visual field is defined as the area that is perceived while fixating one central target. According to traquair’s analogy, visual field is “an island of vision surrounded by a sea of darkness”. It is a 3D hill – peak being fovea and at ground level, it extends ~ 50° superiorly, 60° nasally, 70° inferiorly and 90° temporally.
Normal blind spot is 15° temporal to the fixation and measure 6° wide and 8° high.
Terminologies:
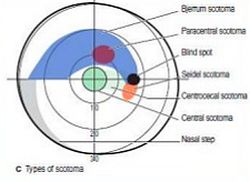
- Scotoma: Area of reduced sensitivity surrounded by a more sensitive area
- Depression: Area of reduced sensitivity without a normal surround
- Isopter: A threshold line joining points of equal sensitivity on a visual field chart
- Fixation: Part of visual field corresponding to fovea centralis
- Central field: Portion of visual field within 30° of fixation
- Bjerrum’s area: Central visual field within 25° of fixation

The normal human optic nerve is made up of 1.0-1.2 million axons of retinal ganglion cells (RGC), which converge at the optic disc. These fibers make up the retinal nerve fiber layer and lie in the inner retina, just below the internal limiting membrane.
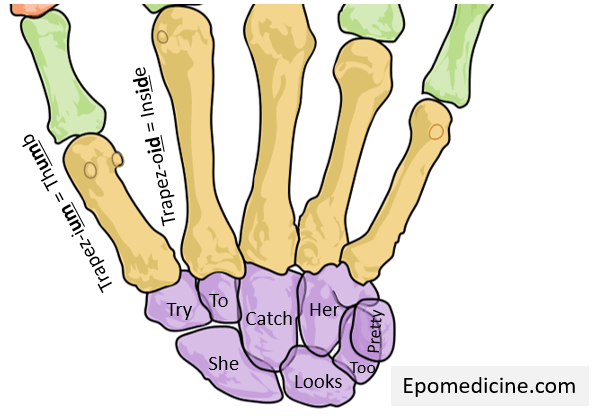
Distribution of retinal nerve fibers:
- Fibers from nasal half of the retina come directly to the optic disc as superior and inferior radiating fibers (srf and irf).
- Fibers from the macular area come horizontally as papillomacular bundle (pmb).
- Fibers from the temporal retina arch above and below the macula and papillomacular bundle as superior and inferior arcuate fibers with a horizontal raphe in between (saf and iaf).
Arrangement of nerve fibers within Optic Nerve Head (ONH):
- Deeper fibers from peripheral retina occupy peripheral or superficial location in ONH
- Superficial fibers from central retina occupy central or deep location in ONH
Note:
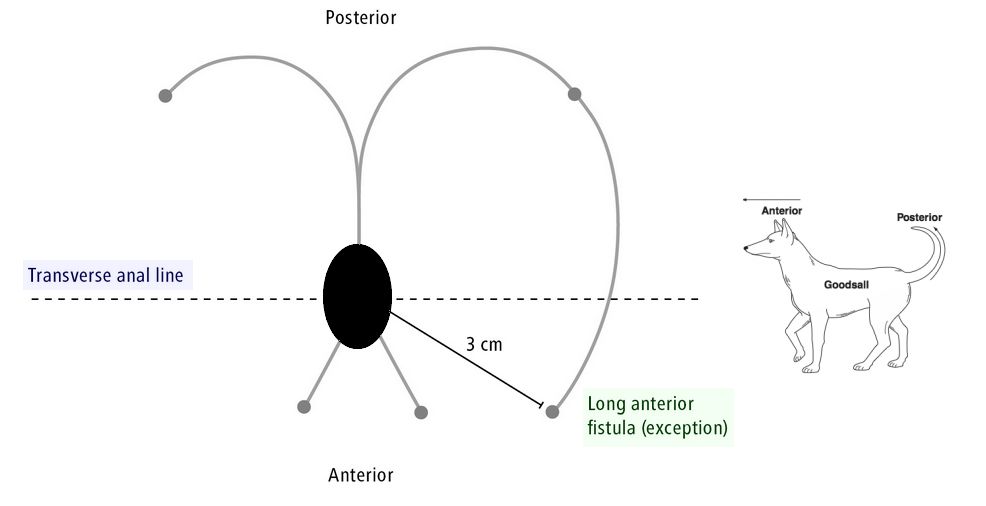
1. Arcuate nerve fibers are the most sensitive to glaucomatous damage and stop at horizontal raphe (nasal step).
Why is arcuate fibers more susceptible or involved earlier?
There is no clear answer to this. We have few hypotheses:
a. The superior and inferior poles of the optic nerve head may be watershed areas at the junction of the vascular supply from adjacent ciliary vessels.
b. Ultrastructural examination of the lamina cribrosa shows that the pores in the superotemporal and inferotemporal areas are larger. The large pores may make these regions more vulnerable to compression.
c. According to Syed S. Hasnain’s temporal sinking hypothesis, circular border tissue keeps the optic disc in place in the scleral canal. Border tissue atrophies due to chronic ischemia either due to high intraocular pressure or due circulatory problems. Due to atrophy of the border tissue the optic disc will start sinking in its entirety. Due to normally temporally tilted disc the temporal fibers consisting of superior and inferior arcuate and centrally located macular fibers will be stretched and severed against the scleral edge due to sinking disc earlier. Arcuate fibers being fewer in number compared to the macular will be depleted earlier giving rise to arcuate field defects.
2. Inferior arcuate fibers are more susceptible resulting in arcuate scotomas earlier in Superior visual field. This can be correlated in Glaucomatous optic disc changes as inferior temporal rim thickening in early stages. The reason behind this still remains obscure.
3. Radiating fibers are more resistant to glaucomatous damage and do not stop at horizontal raphe (temporal wedge defect do not respect horizontal meridian)
4. Macular fibers are the most resistant to glaucomatous damage (retention of central vision till end)
Progression of Visual Field Defects in Glaucoma
90% of the early glaucomatous changes are within central field.
A. Early non-specific changes:
- Isopter contraction (Generalized depression): Mild constriction of central and peripheral field
- Baring of blind spot: Exclusion of blind spot from the central field due to inward curve of the outer boundary of 30° central field
- Peripheral nasal step (may be early or late): Due to unequal contraction of peripheral isopter
- Small wing-shaped Paracentral scotoma (Within Bjerrum’s area): Isolated or associated with nasal step
- Siedel’s sickle-shaped scotoma: Paracentral scotoma joins the blind spot (it is alsko known as Derringer scotoma)
C. Late significant changes:
- Arcuate or Bjerrum scotoma: Extension of Seidel’s scotoma in an area either above or below the fixation point to reach the horizontal line
- Ring or Double arcuate scotoma: When 2 arcuate scotomas join together
Roenne’s central nasal step: Because of the anatomy of the horizontal raphe, all complete arcuate scotomas end at the nasal horizontal meridian. A steplike defect along the horizontal meridian results from asymmetric loss of nerve fiber bundles in the superior and inferior hemifields.
D. Advanced glaucomatous field defects:
- Tubular vision: Only a small island of central vision accompanied by temporal island
- No light perception: Complete visual field defect (temporal island is the most resistant one)
If you have visual or text mnemonic to remember this, do comment or send us via message box or mail.
Submitted by – Sulabh Shrestha

Very educative. Thumbs up.
pnemonic is IC BB Wings & SAD Steps. (i see blackberry wings and sad steps). IC Isopter contraction. BB baring of blind spots. Wings wing shaped scotoma. SAD- S for Seidel’s scotoma. A for arcuate scotoma. D for double arcuate scotoma. Steps roenne’s central nasal steps. and peripheral nasal steps which can appear either as early or late change.
Thank u ,it helped me lot
Thank you it helped me another
More easy and understandable than in text books… Tq.. Pneumonics are too helpful
Very well explained – thanks
Thanks!
Thanks ,very helpful.
I couldn’t understand much…
Thanks alot.. It is simplfied and helpfull..
Why is the temporal island the most resistant one here? I thought macular fibres were more resistant.