Diagnosis and management of a case of parotid enlargement requires systematic approach. Here, I have tried to present a simplified approach to parotid enlargement.
A) DIFFERENTIAL DIAGNOSES OF PAROTID ENLARGEMENT:
- Child: Mumps, Coxsackie
- Adult: S.aureus
2. Non-infectious benign:
- Epithelial: Pleomorphic adenoma, Warthin tumor, Oncocytoma, Monomorphic adenoma
- Non-epithelial: Lymph node, Cysts, Lipoma, Lymphoepithelial lesion, Capillary hemangioma
3. Non-infectious malignant:
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Mixed malignant tumor
- Acinic cell carcinoma
- Adenocarcinoma
- Squamous cell carcinoma
Relevant terms:
- Sialadenitis: Salivary gland inflammation
- Sialolithiasis: Salivary gland/duct calculi
- Sialadenosis: Non-inflammatory, symmetrical swelling usually of parotid, caused by systemic, frequently unknown cause – chronic alcoholism, vitamin deficiency, diabetes, protein deficiency, anorexia nervosa
- Mumps: Acute viral sialadenitis (paramyxovirus)
B) HISTORY FOR PAROTID ENLARGEMENT:
1. Character of Parotid Mass:
- Onset and duration: Rapid (inflammatory) vs slow growing (neoplastic, sialadenosis, chronic sialadenitis)
- Diffuse (sialadenosis, sialadenitis) vs discrete mass (tumor)
- Unilateral (acute bacterial sialadenitis, neoplasm) versus bilateral (sialadenosis, mumps – viral sialedenitis)
- Painful (acute inflammatory, increases with food ingestion – sialolithiasis)
2. Contributing Factors:
- Exposure to radiation or toxins (lead or mercury)
- History of sarcoidosis, Sjögren’s disease, tuberculosis, gout, amyloidosis
- Recent facial trauma, surgery, or dental work
- Immunization history (specifically measles, mumps, rubella [MMR] vaccine)
3. Associated Symptoms and Signs: xerostomia, sialorrhea, weight loss, fever, trismus
C) PHYSICAL EXAMINATION FOR PAROTID ENLARGEMENT:
1. Differentiate if the mass is intra-parotid or extra-parotid: A parotid mass has following characteristics –
- Swelling from front, below and behind the ear
- Raises ear lobule
- Retromandibular groove obliterated
- When palpated and rolled over styloid and under mandible – not freely mobile and doesn’t move below mandible
2. Assess if the deep lobe of parotid is involved or not (involved in malignancy):
- Facial nerve (CN VII) involvement
- Tonsil deviation medially
- Bimanually palpable
3. Fixity – to skin or masseter (malignancy)
4. Tenderness (inflammatory)
5. Expression from Stensen’s duct – Pus (parotitis) and Blood (malignancy)
6. Deep cervical lymphadenopathy (malignancy)
7. Soft/firm (benign) vs Hard/fixed (malignant)
Notes: Masseter hyperplasia can mimic parotid enlargement and is differentiated by having the patient to squeeze the jaws together which leads to activation of masseter muscle allowing for access to inspection and palpation.
D) DIAGNOSTIC STUDIES FOR PAROTID ENLARGEMENT:
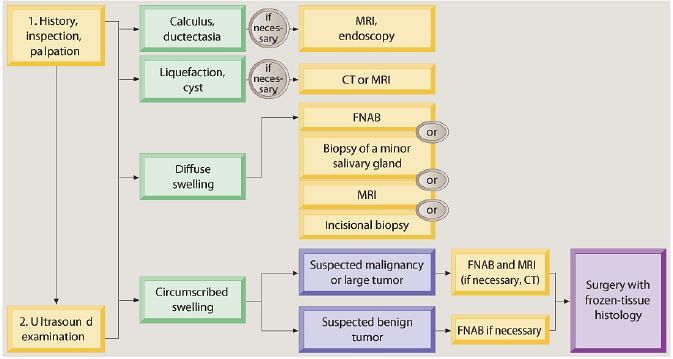
1. Ultrasonography (USG):
- 1st choice of imaging study
- can differentiate normal glandular parenchyma, inflammatory process (with or without liquefaction),cystic lesions, tumors, lymph nodes and calculi
- not good for evaluating deep lobe of parotid
2. CT/MRI (MRI is superior):
- When clinical examination and ultrasonography is non-yielding
- Evaluating size, nerve and deep lobe involvement
- Node involvement
- Preoperative evaluation
3. FNA:
- For discrete nodules of the parotid gland
- Differentiates cysts, inflammatory processes, lymphoma, and other neoplasms
- Preoperative histologic diagnosis
- Predicting extent of surgery
4. Plain X-ray:
- Not much helpful
- Sialolithiasis: must have high calcium content and must be atleast 2-3 mm
- Malignancy: bone resorption
5. Open Biopsy:
- Incisional biopsy/enucleation (without identifying facial nerve):
- risks tumor seeding, recurrence, facial nerve injury, and violation of tumor margins
- contraindicated in benign tumors
- Superficial/total parotidectomy (with facial nerve identification) with intraoperative frozen section: typically required
6. Technetium-99m Isotope Scan:
- Rarely utilized
- May differentiate a Warthin’s tumor and oncocytoma from other salivary gland neoplasms
7. Sialography:
- Visualizes ductal anatomy
- Indicated for ductal calculi, trauma, fistulas, Sjögren’s disease
- Contraindicated in acute infections
8. Sialendoscopy:
- Can demonstrate mucus plugs, calculi and stenoses
- Interventional procedures like dilation or stone removal by loop or laser lithotripsy
9. Labs: may consider mumps titers, CBC, autoimmune and Sjögren’s profile (SS-A, SS-B, ANA, ESR)
E) TREATMENT FOR CAUSE OF PAROTID ENLARGEMENT:
1. Acute Sialadenitis:
- Rehydration
- Warm compresses
- Antimicrobial therapy (may require parenteral antibiotics for severe cases)
- Sialagogues (e.g. Pilocarpine)
- Salivary gland massage
- Oral irrigations
- If no resolution after 2–3 days then consider CT or USG to evaluate for abscess (may require I&D)
2. Sialolithiasis:
- Gland massage
- Bimanual expression
- Transoral incision
- Sialodochoplasty (reconstruct duct)
- Gland excision if recurrent or if stone is lodged within substance of the gland
3. Epithelial lesions:
- Step 1: Superficial parotiectomy
- Step 2: Frozen section
- Step 3:
- Benign: Stop
- Malignant – Low/Intermediate grade: Total parotidectomy with CN VII preservation
- Malignant – High grade: Extended or Radical parotidectomy with CN VII resection and Modified radical neck dissection
- CN VII impaired and unseparable from tumor: Nerve excision followed by attempt of immediate grafting
- Step 4: Postoperative radiotherapy for malignancy
Note: Warthin tumor can be treated by enucleation.
Prognosis: Low grade mucoepidermoid carcinoma > Acinic cell carcinoma > High grade mucoepidermoid carcinoma > Malignant mixed tumor > Adenoid cystic carcinoma > Squamous cell carcinoma
Indications of neck dissection: Clinically apparent cervical lymphadenopathy, tumors > 4 cm (risk of occult metastases > 20%), high grade histology (occult metastases > 40%)
Elective neck dissection for adenoid cystic carcinoma is not recommended (low risk of occult nodal metastases)For parapharyngeal space extension: Parapharyngeal space (Infratemporal fossa) dissection
F) PRINCIPLES OF PAROTIDECTOMY
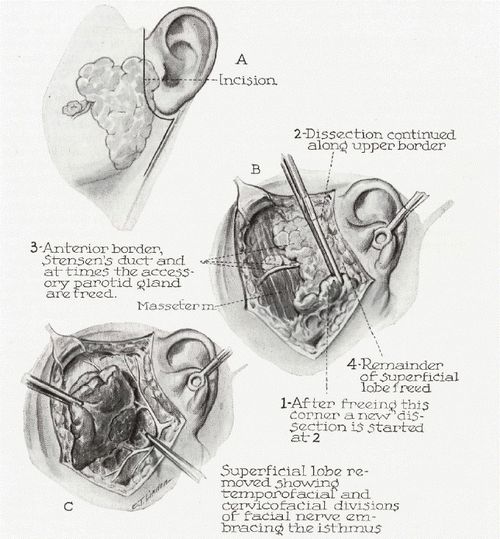
1. Superficial/Lateral Parotidectomy:
- Indication: diagnostic and therapeutic excision of benign or malignant tumors that involve the superficial lobe of the parotid only
- Typically preserves facial nerve
- Resects majority of parotid gland lateral to facial nerve
- Facial Nerve Markers
- Anesthesia: General anesthesia
- Incision: Preauricular and Submandibular lazy-S incision (Blair’s incision)
- Ligation of greater auricular nerve is mandatory to prevent neuroma formation
2. Total Parotidectomy:
- Indications: high-grade malignancy or deep lobe or facial nerve involvement
- Excision of both superficial and deep lobe with preservation of facial nerve
- Extended total parotidectomy: Excision of facial nerve may be indicated for malignant tumors (encasement or invasion of facial nerve)
- Resection of retromandibular vein by ligation is mandatory to clear the retromandibular space
- Can be done by transcervical approach
Subtotal parotidectomy: Lateral parotidectomy, somewhat medial to the facial plexus, but not necessarily including deep portion, under preservation of facial nerve.
3. Radical Parotidectomy: includes possible mandibulectomy, petrosectomy, periglandular skin, or facial nerve, indicated for aggressive malignant disease
- Removal of: duct, masseter fibers, buccinator, pterygoid
Parotidectomy Complications:
- Facial Nerve Paresis/Paralysis: should be repaired immediately
- Hypesthesia of Greater Auricular Nerve: usually resolves within 9 months if not deliberately transected
- Salivary Fistula: uncommon, usually spontaneously resolves in 2–3 weeks; Rx: probe wound to release fluid (aspiration), pressure dressing, surgical closure for prolonged drainage (may consider tympanic neurectomy)
- Other Complications: hematoma, infection, flap necrosis, trismus, seroma, and recurrence
- Frey’s Syndrome (Gustatory Sweating):
- Pathophysiology: injury to the auriculotemporal nerve (sympathetic fibers) results in aberrant innervation of cutaneous sweat glands (which share the same neurotransmitter) by postganglionic
parasympathetic fibers - may occur up to 5 years postoperatively
- less incidence with the use of “thick” skin flaps or placement of dermal grafts or allograft under skin flap
- Symptoms: sweating and reddening of skin during meals
- Investigation: Starch iodine test (Iodine + Sweat = Blue color)
- Management:
- Medical Management: antiperspirant (aluminium chloride) and anticholinergic preparations (scopolamine, glycopyrrolate, diphemanil methylsulfate), Botox injections
- Surgical Management: tympanic neuronectomy (Jacobson’s nerve section via tympanotomy approach, controversial) high incidence of recurrence, interpose a sheet of fascia lata or dermis
between skin and parotid gland - Radiation Therapy: reserved for failed management with severe symptoms
- Pathophysiology: injury to the auriculotemporal nerve (sympathetic fibers) results in aberrant innervation of cutaneous sweat glands (which share the same neurotransmitter) by postganglionic
Difference between 2 common benign tumors:
| Pleomorphic adenoma | Warthin tumor (Adenolymphoma) | |
| Incidence | 70-80 % | 10% |
| Gender/Age | F>M; 40s | M>F; smoker; middle age/elderly |
| No./Site | Single/Unilateral | May be multiple/bilateral |
| Consistency | Nodular/Firm | Smooth, soft, cystic |
| Histology | Pleomorphism | 2 layer epithelium and lymphoid tissue |
| 99m Tc scan | Cold spot | Hot spot |
| Treatment | Superficial parotidectomy | Enucleation |