Red eye reflects hyperemia or engorgement of superficial visible conjunctival, episcleral or ciliary vessels.
A) DIFFERENTIAL DIAGNOSES FOR ACUTE RED EYE
1. Painless red eye:
- Lids normal: Conjunctivitis
- Lids abnormal:
- Blepharitis
- Ectropion
- Trichiasis
- Eyelid lesion
b) Localized redness:
- Pterygium
- Corneal foreign body
- Ocular trauma
- Subconjunctival hemorrhage
- Episcleritis
2. Painful red eye:
a. Cornea abnormal:
- Herpes simplex keratitis
- Bacterial/Acanthamoebal ulcer
- Marginal keratitis
- Foreign body/Corneal abrasion
b. Lids abnormal:
- Chalazion
- Blepharitis
- Herpes zoster
c. Diffuse Conjunctival congestion:
- Viral conjunctivitis
- Allergic conjunctivitis
- Bacterial conjunctivitis
- Dry eyes
d. Ciliary congestion:
- Angle closure glaucoma
- Anterior uveitis (Iridocyclitis)
e. Scleral congestion:
- Scleritis
B) HISTORY AND EXAMINATION FOR ACUTE RED EYE:
Perform systematic ocular history and examination with special emphasis on:
Step 1: Assess for possible causes of red eye
- Trauma (foreign body, subconjunctival hemorrhage)
- Recent ocular history such as surgery (postoperative endophthalmitis)
- Previous history of Angle closure glaucoma, uveitis or systemic illness
Step 2: Painful or painless red eye ?
Step 3: If the pain is deep – assess for pattern of redness
a. Diffuse: Examine eyelids
- Lids normal: Rule out scleritis
- Lids abnormal:
- With ptosis: Orbital cellulitis, Grave’s disease
- Without ptosis: Grave’s disease
b. Focal: Scleritis
c. Ciliary: Examine pupils
- Mid-dilated: Acute angle closure glaucoma
- Small or normal pupils: Evaluate anterior chamber
- Cloudy: Evlauate cornea
- Cornea clear: Anterior uveitis
- White infiltrate: Corneal ulcer
- Layered WBCs: Hypopyon
- Layered RBCs: Hyphema
- Cloudy: Evlauate cornea
Step 4: If the pain is superficial – Assess vision
a. If decreased vision – Perform topical fluorescein staining
- Foreign body
- Chemical injury
- Corneal abrasion
- Corneal ulcer
b. If normal vision – Evaluate pattern of redness
- Diffuse congestion: Examine lids
- Abnormal: Blepharitis, Chalazion, Hordeolum
- Normal: Note the type of discharge
- No discharge: Non-specific conjunctivitis
- Purulent: Bacterial conjunctivitis
- Watery: Is itching present?
- No itching: Viral conjunctivitis
- Itching: Allergic conjunctivitis (Medication related or unrelated)
- Focal: Is conjunctival lesion present:
- Conjunctival lesion present: Pingueculum, Pterygium
- Conjunctival lesion not present: Subconjunctival hemorrhage, Episcleritis
Step 5: If there’s no pain but the vision is poor – possible causes are
- Vasculitis
- Vitreitis
- Retinitis
| Cause of red eye | ||||||
|---|---|---|---|---|---|---|
| Feature | Conjunc-tivitis | Sub- conjun-ctival hemor-rhage | Keratitis | Iritis | Acute angle closure glaucoma | Scleritis |
| Conjes-tion | Diffuse, unilateral or bilateral | Unilateral, not truly injected but rather discrete confluent change | Ciliary pattern,unilateral | Ciliary pattern, unilateral | Ciliary pattern, unilateral | Localised, unilateral |
| Cornea | Clear | Clear | Hazy, localised opacity (infiltrate), epithelial defect (fluorescein positive) | May be hazy | Hazy, iris detail indistinct | Clear |
| Pupil | Unaffected | Unaffected | Unaffected (unless secondary uveitis present) | Constricted, poor light response, may be distorted | Fixed, mid-dilated | Unaffected (unless secondary uveitis present) |
| Vision | Generally unaffected | Unaffected | Moderately to severely reduced | Mildly to moderately reduced. | Severely reduced, blurred, possible coloured halos around lights | May be reduced |
| Disch-arge | Yes; purulent more likely with bacterial, watery more likely with viral | Minimal (watery) | Yes; usually watery | Minimal (watery) | Minimal (watery) | Minimal (watery) |
| Pain | Yes; gritty or stabbing pain | Generally none | Yes; usually severe | Yes; moderate to severe | Yes; usually severe (with vomiting and headache), globe tender and hard if palpated | Moderate to severe (described as deep pain), localised significant tenderness |
| Photo-phobia | No | No | Yes | Yes | Sometimes | Sometimes |
Diagnostic aids for acute red eye:
- Light sensitivity: Iritis, keratitis, abrasion, ulcer
- Unilateral: Above + herpes simplex, acute angle closure glaucoma
- Significant pain: Above + scleritis
- White spot on cornea: Corneal ulcer
- Blurred vision: All of the above
- Non-reactive pupil: Acute glaucoma, iritis
- Copious discharge: Gonococcal conjunctivitis
- Blurred vision: All of the above
C) MANAGEMENT OF CAUSES OF RED EYE:
1. Orbital cellulitis:
- lid erythema, proptosis, and restricted eye movements, pseudoptosis secondary to the swelling, fever, anorexia, malaise, eyelid and periocular pain, with swelling, double/blurred vision
- may give a history of sinusitis or preseptal celluitis
- treatment:
- Hospital admission
- Send for CBC and blood cultures
- Urgent CT: to rule out associated abscess
- IV antibiotics: likely organisms are Strep. pyogenes, Strep. pneumoniae, Staph. aureus
i.v. Ceftriaxone 50 mg/kg/dose (2g) iv 12H
and
i.v. flucloxacillin 50 mg/kg/dose 6-hourly (maximum 2 g/dose). - If abscess is present: Surgical drainage of an abscess
2. Scleritis:
- Eye pain: severe, deep, boring in nature; disturbs sleep; radiate to the eyebrow, forehead or jaw; exacerbated by eye movements. Minimal and temporary relief of pain from analgesics.
- Epiphora, Photophobia, Tender globe, Nausea/vomiting, Redness of the eye, may complain of reduced vision
- Examination in daylight – the sclera may appear red/blue. There will be injection of deep episcleral vessels that do not blanch on phenylephrinene (10% drop) instillation. There may be areas of scleral translucency (blue tinged) indicating thinning due to previous episodes of scleritis. A severe necrotizing form of scleritis would be indicated by black or brown areas. An area of central whiteness indicates that this area has become avascular.
- Slit lamp examination – corneal/intraocular inflammation. Thickened oedematous sclera.
- 50% of cases are associated with an underlying systemic condition – autoimmune diseases, arthritis, vasculitis and infections like TB, syphilis, varicella zoster (Look for underlying systemic disease)
- More common in women with peak incidence in 50s.
- Treatment
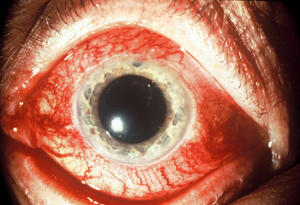
3. Acute Angle Closure Glaucoma:
- History: Severe eye pain, nausea, vomiting, (may misleadingly present as an acute abdomen), headache, red eye, rainbow halos around lights, decreased vision. There may be a preceding history of intermittent blurred vision, and halos around lights, for example after an evening in a dark environment, due to transient closure of the irido-corneal angle caused by pupil dilation.
- Eamination: Poor visual acuity, red eye (ciliary flush), cloudy cornea (secondary to corneal oedema), fixed and mid-dilated oval shaped pupil, eye that is stone hard on palpation, shallow anterior chamber, RAPD – if optic nerve damage has occurred
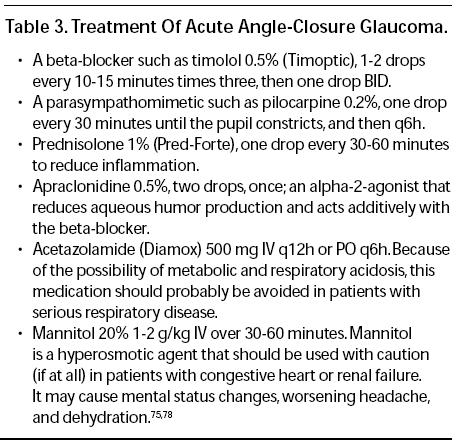
- Treatment:

4. Anterior uveitis (Acute iridocyclitis):
- History: Photophobia (due to reactive spasm of inflamed iris muscle), ocular pain, tenderness of the globe, brow ache (ciliary muscle spasm), decreased VA (in severe cases with hypopyon), lacrimation
- Examination:
- Ciliary flush (perilimbal conjunctival injection), miosis (spasm of sphincter muscle)
- Anterior chamber “cells” (WBC in anterior chamber due to anterior segment inflammation) and “flare” (protein precipitates in anterior chamber 2° to inflammation)
- Hypopyon (collection of neutrophilic exudates inferiorly in the anterior chamber)
- Occasionally keratic precipitates (clumps of cells on corneal endothelium)
- Typically reduces IOP because ciliary body inflammation causes decreased aqueous production; however, severe iritis, or iritis from herpes simplex and zoster may cause an inflammatory glaucoma (trabeculitis)
- Look for arthritis, back pain, signs of tuberculosis and coexisting medical conditions such as ulcerative colitis
- Treatment: Severity of anterior uveitis can be graded based on severity of symptoms, decrease in visual acuity, depth of circumcorneal flush, density of KPs, flare reaction and rise in IOP
- Mydriatics/Cycloplegics: Cyclopentolate, 1% (t.i.d.) or homatropine, 5% (b.i.d.-t.i.d.) or atropine 1% (bid-tid)
- Relieves pain by immobilizing iris
- Prevents synechiae formation
- Stabilize blood-aqueous barrier and decrease flare reaction
- Steroids (Anti-inflammatory): Prednisolone, 1% (b.i.d.-q.i.d.) or Fluoromethalone 0.1% and 0.25%
- NSAIDs: Oral aspirin or ibuprofen or flurbiprofen, 2 tablets (q.4h)
- Consider beta blockers if IOP is elevated
- Use dark glasses
- Re-evaluate after 5-7 days (or sooner if severe) or p.r.n
- Mydriatics/Cycloplegics: Cyclopentolate, 1% (t.i.d.) or homatropine, 5% (b.i.d.-t.i.d.) or atropine 1% (bid-tid)
6. Ocular foreign body:
If the patient was working with metal or wood, inspect the eye for a foreign body.
- History: Sudden discomfort in eye, Reflex blinking due to foreign body sensation, irritation and gritty feeling if the foreign body , lacrimation and photophobia are present in cases of corneal involvement.
- Examination: reflex blepharospasm, foreign body is visible on the bulbar conjunctiva, limbus, cornea, sulcus subtarsalis and fornix by the naked eye, oblique illumination with a loupe or slit-lamp examination.
- Treatment:
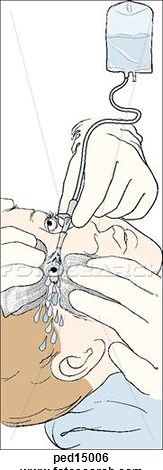
- Step 1: Instil local anesthetic eyedrops
- Step 2: Irrigation of eye
- Position: sitting or lying down with neck and shoulders covered with waterproof sheet; head tilted towards affected side with kidney dish against cheek
- Fill irrigating fluid: Fill the feeding cup with the irrigating fluid and test it for temperature by pouring a small amount against the patient’s cheek
- Fix the gaze: Ask the patient to fix his/her gaze ahead
- Retract eyelids: Spread open the eyelids, if necessary using eyelid retractors
- Irrigate: Pour the fluid slowly and steadily, from a distance of no more than 5 centimetres, onto the front surface of the eye, and importantly, inside the lower eyelid and under the upper eyelid
- Evert the upper eyelid to access all of the upper conjunctival fornix
- Ask the patient to move the eye continuously in all directions while the irrigation is maintained for at least 15 minutes (30 minutes is better)
- Remove any residual foreign bodies with moist cotton buds or forceps
- Check and record the visual acuity when the procedure is finished
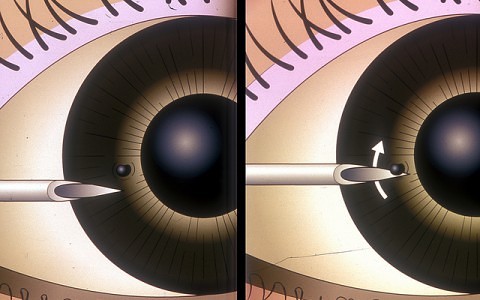
- Step 3: For embedded corneal foreign body

- Instill fluorescein dye
- Ask the patient to look straight ahead, fix gaze and keep perfectly still
- With one hand, gently control the patient’s eyelids
- With the other hand, support the sterile needle with two fingers and the thumb
- Approach the cornea slowly with the bevel of the needle uppermost and horizontally ‘flat on’ to the cornea (tangential approach to prevent corneal perforation)
- Gently lift off the foreign body (FB) from the corneal surface using lever movement.
- Check the patient’s eye, carefully everting the upper eyelid to ensure no FB’s remain – a corneal abrasion may be seen
- If metal is lodged in the cornea for more than four to six hours, rust will begin to form in the adjacent tissue. This is typically seen as a brownish-orange ring that appears to feather into the surrounding tissue. Although the rust ring can occasionally be lifted in its entirety with a jeweler’s forceps, an Alger brush will be required in the vast majority of cases to free the area of rust.
- Instill antibiotic ointment and apply a firm eye dressing, using two pads and a bandage, for 24 hours
- Step 4: Follow up next day
- Look for infection, iritis and recurrent corneal erosion.
7. Chemical injury of eye:
- Immediately irrigate at site of accident with water or buffered solution IV drip for at least 20-30 min with eyelids retracted in emergency department
- Swab upper and lower fornices to remove possible particulate matter
- Do not attempt to neutralize because the heat produced by the reaction will damage the cornea
- Cycloplegic drops to decrease iris spasm (pain) and prevent 2° glaucoma (due to posterior synechiae formation)
- Topical antibiotics and patching
- Topical steroids to decrease inflammation, use for less than 2 wk (in the case of a persistent epithelial defect)
8. Eyelid lesions:
Diagnosis:
- Crusting: Blepharitis
- Towards eyelid margin; pus point: External hordeolum/stye
- Away from eyelid margin; lumpy mass: Chalazion
Treatment:
- Warm compresses (for 5 minutes) applied to the lids:
- can increase oil production and melt the oil in the meibomian glands
- use of a warm washcloth to apply heat
- Eyelid scrub hygiene:
- to remove eyelash debris, bacteria, bacteria toxins, oil and scurf
- use a cotton earbud soaked in baby shampoo or modern methods like foam, gel and pre-moistened pads such as Ocusoft Eyelid Cleanser
- Mechanical glandular eyelid massage:
- to facilitate the flow of the meibomian oil from the glands
- applying light pressure with a fingertip or a Q-Tip to the lid margin near the base of the lashes
- Artificial Lubricants:
- such as Ocusoft, re-lube, etc.
- Topical (drops and ointments) antibiotics
- Non-resolving:
- Chalazion: Intralesional steroid or Incision and currettage
- Stye (if abscess formed): Drain by pulling out eyelash or Incision
- Blepharitis:
- Topical corticosteroids (for < 2 weeks)
- Others: Diet rich in Omega-3 fatty acids (fish, flax seed and walnuts)
11. Conjunctivitis:
a. Viral conjunctivitis:
- Simple follicular conjunctivitis – supportive; cold compresses over the eyelids or artificial tears may provide some symptomatic relief. Strict hygiene must be emphasized, e.g. hand washing, avoiding close contact, not sharing towels.
- Molluscum contagiosum: nodules can be excised.
- Herpes simplex infection: topical aciclovir
- Followup
b. Allergic conjunctivitis:
- Eliminate underlying cause (allergen)
- Topical antihistamine and/or mast cell stabilizing drops
- Follow-up is indicated only if symptomatic treatment is ineffective.
c. Bacterial conjunctivitis:
- Gonococcus causes hyperacute puruplent conjunctivitis and is potentially sight threatening and requires urgent workup and treatment.
- Less virulent: Streptococcus pneumoniae, Haemophilus influenzae, and Chlamydia
- Intitially empiric therapy: Broad-spectrum antibiotics like Ofloxacin (Exocin eye drops), Ciprofloxacin (Cipro-cent) eye ointment
- Later specific therapy based on culture sensitivity
12. Pterygium and Pignguecula:
- Pinguecula is an elastotic degeneration of conjunctiva that never encroanches cornea while Pterygium is a fibrovascular conjunctival growth that encroaches towards the cornea
- Hence, pterygium may cause astigmatism and diplopia
- Usually managed conservatively with artificial lubricants and uv protective glasses
- Antibitoics and steroids can be used if inflamed
- Pterygium excision may be indicated in some cases
REMEMBER THE RED FLAGS! IN ACUTE RED EYE
- Severe eye pain
- Severe photophobia
- Marked redness of one eye (Unilateral)
- Reduced visual acuity (after correcting for refractive errors)
- Suspected penetrating eye injury
- Worsening redness and pain occurring within one to two weeks of an intraocular procedure (Suspected endophthalmitis)
- Irritant conjunctivitis caused by an acid or alkali burn or other highly irritating substance
- Purulent conjunctivitis in a newborn infant
I enjoyed theses slides, my life made easier to understand. Keep up with the gud work
Excellent work