Synonyms: Rosacea acne, Adult acne, Rhinophyma
Defintion: A chronic and recurrent inflammatory disorder of the pilosebaceous units and vasculature of the face characterized by erythema and telangiectases and punctuated by acute episodes of papules, pustules and swelling.
Rosacea is a disorder of sebaceous gland. Learn the anatomy and physiology of sebaceous gland.
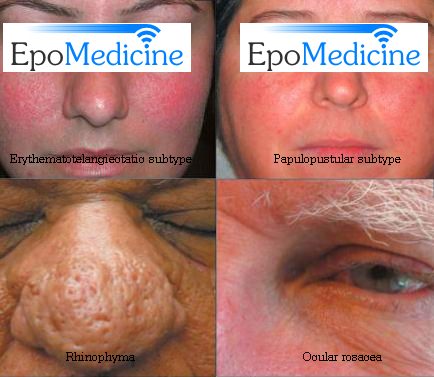
Classification:
- Erythematotelangiectatic subtype (persistent centrofacial erythema and extenisve history of prolonged flushing)
- Papulopustular subtype (resembles acne vulgaris but lacks comedones)
- Phymatous subtype (thickened skin and irregular surface eg. rhinophyma of nose)
- Ocular subtype (blepharitis, conjunctivitis, keratitis)
Etiopathogenesis: Unknown
- Vascular abnormalities: Often seen in those who flush easily to heat, spicy food, drinking hot liquids alcohol, stress
- VEGF (Vascular endothelial growth factor) may have a role
- Suspected micro-organisms: Demodex folliculorum, Bacillus oleronius and Helicobacter pylori
- Other theories:
- Inflammation and dermal matrix degeneration leading to a weakened support structure for cutaneous vasculature
- Prolonged exposure to UV radiation
- Pilosebaceous unit abnormalities
- Age: Usually adults; peak incidence in 30s and 40s
- Gender: Female > Male
- Race: More prevalent in fair-skinned individuals
- Convex surface of central face like cheeks, chin, centre of forehead, nose
- Involvement in symmetrical
- Periorbital and perioral areas are spared
- Intermittent flushing is followed by a fixed erythema and telangiectasia.
- Discrete dome shaped inflamed papules, papulopustules and, rarely nodules develop later.
Complications:
- Ophthalmologic: Blepharitis, conjunctivitis, keratitis
- Rhinophyma: More common in males; caused by hyperplasia of sebaceous glands and connective tissue of nose
- Lymphedema: Infraorbital and forehead
- Rebound flare of pustules: on stopping treatment with topical steroids
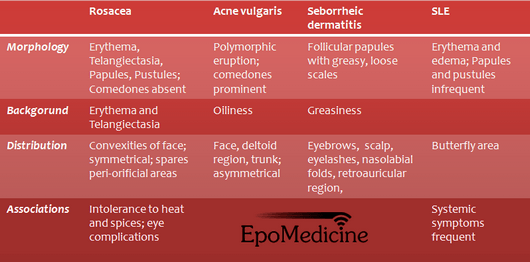
Differential diagnosis:
Rosacea should be distinguished from:
- Acne vulgaris: in which there are comedones (blackheads), a wider distribution, and improvement with sunlight.
- Seborrhoeic eczema: in which there are no pustules and eczematous changes are present.
- Systemic Lupus erythematosus (SLE): which shows light sensitivity, erythema, and scarring but no pustules.
- Perioral dermatitis: which occurs in women with pustules and erythema around the mouth and on the chin. There is usually a premenstrual exacerbation.
Treatment:
Agents generally appropriate for the treatment of both rosacea and acne vulgaris:Topical: Clindamycin, Retinoids, Azelaic acid, Sulfur, Sodium sulfacetamideOral: Tetracyclines, Azithromycin, IsotretinoinAgents generally appropriate for the treatment of rosacea but, not acne vulgaris:Topical: Metronidazole, Tacrolimus, PimecrolimusOral: MetronidazoleAgents generally appropriate for the treatment of acne vulgaris, but not rosacea:Topical: Benzoyl peroxide, Salicylic acidOral: Trimethoprim-sulfamethoxazole
A) Topical:
- Sunscreens
- Metronidazole 0.75% gel or cream
- Retinoic acid 0.025%
- Pimecrolimus 1% and tacrolimus 0.03% and 0.1% ointment
B) Systemic:
Needed in cases of acute exacerbations and severe rosacea
- Antibiotics: Long term courses of Tetracycline or Erythromycin; Metronidazole (For stubborn rosacea)
- Tetracycline dosage: Courses should last for at least 10 weeks and, after gaining control with 500–1000 mg daily, the dosage can be cut to 250 mg
- Isotretinoin (For stubborn rosacea)
C) Lifestyle change: Avoiding hot and spicy food may help
D) Others: Since the above listed medications suppress papules and pustules but not erythema and telangiectasia, following may be needed –
- Lasers for telangiectases
- Plastic surgery or laser for rhinophyma
- Camoflauge makeup for erythema
- Avoid topical steroids as withdrawl can exacerbate papules and pustules
- Do not prescribe a tetracycline for children and pregnant women
- Oxytetracycline must be taken on an empty stomach half an hour before meals
Mnemonic for medical students: ROSACEAR elapsing remitting facial disorderO ften precedes the development of fixed erythema (chin, nose, cheeks, forehead)S welling and soft tissue overgrowth of the nose (rhinophyma) may occurA void excessive sun exposureC hronic flushing triggered by spicy food, alcohol and high emotionE ye problems like blepharitis, conjunctivitis, keratitisA ntibiotics used during flare ups