Types of Transplant Rejection
| Type | Time | Mechanism | Pathology | Hypersensitivity | Management |
|---|---|---|---|---|---|
| Host against Graft (Host vs Graft) | Mnemonic: TIA | ||||
| Hyperacute | Immediate (<5 days) | Anti-donor antibodies in recipient | Thrombosis and Obliteration of blood supply | Type II | Untreatable Prevent by cross-matching Remove graft |
| Acute (most common) | < 6 months (most common in 1st month) | Anti-donor T cell proliferation in recipient | Interstitial lymphocyte infiltrate | Type IV | Prevent/reverse with immunosuppressants |
| Chronic | Months to years (usually >6 months) | Development of multiple cellular and humoral immune reactions to donor vasculature | Arteriosclerosis and intimal fibrosis | Type III and IV | Unresponsive to immunosuppressants |
| Accelerated acute | First few days (7-10 days) | Activation of memory T and/or B lymphocytes in pre-sensitized receipients (post-formed CMI and antibodies) | May be responsive to antibody therapy: OKT3, ATG |
Post-renal transplant fluid collections
Mnemonic: HEAL
1. Hematoma (Immediate)
2. Encapsulated urine collections/urinomas (1-2 weeks): commonest cause is ureter tip necrosis and may require revision anastomosis
3. Abscess (3-4 weeks)
4. Lymphocele (2 months)
Post-renal transplant renal injury
Mnemonic: SCRI
1. Structural causes: USG
- Renal artery thrombosis – Sudden complete loss of urine output (T/t: Immediate surgery within 30 minutes)
- Renal artery stenosis – Uncontrolled hypertension; allograft dysfunction and edema (T/t: Angioplasty)
- Renal vein thrombosis – Pain and swelling of graft site, hematuria and oliguria (Graft is usually lost)
2. Calcineurin inhibitor toxicity: Cyclosporin level
3. Rejection and/or Recurrence of primary disease: Biopsy (rejection type; MCGN>IgA nephropathy>FSGS)
4. Infection: PCR
- 1-6 months post-transplant: BK virus, CMV
- >6 months post-transplant: PTLD (Post-transplant lymphoproliferative disorder) – EBV
Outcomes
| Transplant | 1 year survival | 5 year survival |
|---|---|---|
| Renal | 90% | 65% |
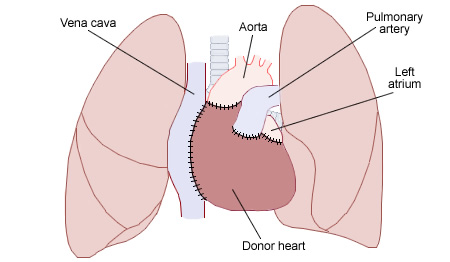
| Cardiac | 80% | 65% |
| Hepatic | 80% | 55% |
| Lung | 70% | 55% |
| Pancreatic | 75% | |
| Small bowel | 60% |
Immunosuppressants
| Drugs | Mechanism | Adverse effects |
|---|---|---|
| Corticosteroids | Suppress all inflammatory elements of immune response | ‘Cushingoid’ effects |
| Calcineurin inhibitors (Cyclosporin, Tacrolimus) | Suppress T-cells and inhibit IL-2 release | Nephrotoxicity (more with cyclosporin) Diabetes (with tacrolimus) |
| Anti-proliferatives (methotrexate, azathioprine, mycophenolate) | Prevent cell mediated cell mitosis and amplification of response | Renal and hepatic dysfunction, marrow suppression |
| mTOR inhibitors (sirolimus, rapamycin, everolimus) | Prevents T cell and B cell activation by blocking IL-2 receptors | Interstitial pneumonitis |
| Biologic effectors | Basiliximab: anti-IL2-receptor antibody Rituximab: anti-CD20 antibody | Cytokine release syndrome |
| Hydroxychloroquine (for chronic GVHD) | Inhibits antigen processing | Visual disturbances |
| Thalidomide (for chronic GVHD) | Inhibits T-cell function and migration | Sedation, constipation, teratogenicity |
very informative , precise and concise, relevant information