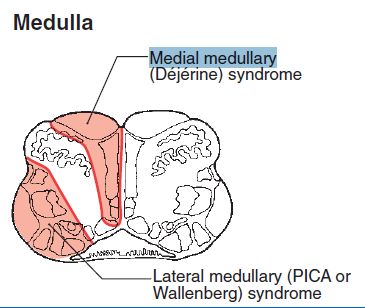
As already discussed in the previous section about Lateral Medullary (Wallenberg) Syndrome:
- 6 “S” pass/lie on the Side (latetral) of Medulla
- Except the anteromedian part supplied by vertebral artery, rest of the medulla is supplied by PICA
Let us now review the relevant anatomy and physiology of the medial portion of medulla in an easy fashion using a mnemonic.
4 “M” represents the 4 Midline or Medial structures
1. Motor pathway (Corticospinal tract)
- Originate in precentral gyrus of frontal lobe and pass through ventral aspect of brainstem
- Lateral corticospinal tract: 90% fibers decussate at the medullary pyramids before entering the cervical cord as lateral corticospinal tract (necessary for fine motor)
- Anterior corticospinal tract: Remaining 10% fibers descend in the ipsilateral spinal cord as Anterior corticospinal tract and ultimately crosses later at the level of spinal cord (necessary for gross motor)
2. Medial lemniscus
- Posterior column donot cross midline: Gracile (medial and carries information from T6 and below) and cuneate (lateral and carries information from above T6 and face) fasciculus in spinal cord
- somatotropic orientation: medial-lateral (leg-arm i.e. – –)
- Decussation as internal arcuate fibers: posterior column now become medial lemniscus
- somatotropic orientation: anterior-posterior (leg-arm i.e. ‘,)
- Medial lemnsicus: After decussation, internal arcuate fibers become medial lemniscus and ascend to enter Ventral postero-lateral (VPL) nucleus of thalamus
- somatrotropic orientation: flips back to medial-lateral (arm-leg i.e. – –)
The somatotropic orientation rotates in a clockwise direction from down to up.
It is responsible for carrying static sensory proprioception (joint-position sensation, two-point discrimination, vibratory sensation) and pain and temperature sensation.
3. Medial longitudinal fasciculs
- Carries ascending fibers from the contralateral interneurons of the abducens nucleus to the ipsilateral oculomotor nucleus (vestibulo-ocular pathway)
- It plays role in conjugate horizontal eye movement
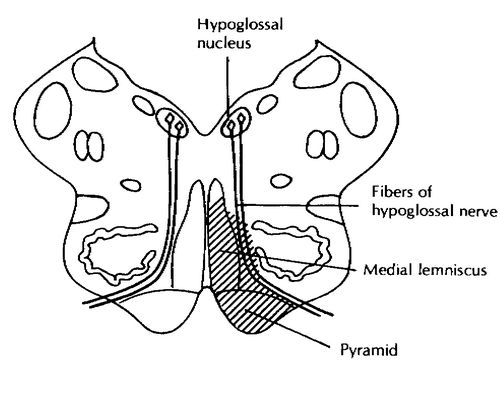
4. Motor nucleus of hypoglossal nerve
- Hypoglossal nerve pass ventrally through the medulla and exit between the inferior olive, laterally, and the medullary pyramid, medially – crosses the premedullary cistern and traverse the skull base through the hypoglossal canal.
- It runs near the internal carotid artery and carotid bulb as it descends in the medial nasopharyngeal carotid space
- Supplies intrinsic and extrinsic muscles of tongue except palatoglossus which is innervated by vagus nerve (CN X)
- The supply is bilateral except for genioglossus which receives only contralateral innervation
- Genioglossus is directed in opposite direction – hence, on protrusion pushes the tongue to the opposite side (i.e. towards dysfunctional genioglossus) – this means, there is neural lesion towards the deviation of tongue (genioglossus receives only contralateral innervation)
- Also innervates the muscles of floor of mouth and upper hyoid musculature (geniohyoid and thyrohyoid)
Note: Purely cranial motor nuclei lie medially and the mixed lie laterally. These pure motor nuclei can divide 12 exactly i.e. 3, 4, 6, and 12. Since, the Cranial nerve 3, 4 and 6 lie above medulla – Cranial nerve 12 is the involved structure.
Now, let us move onto the discussion of medial medullary syndrome (Djerine’s syndrome):
Cause of Medial medullary (Djerine’s) syndrome
Vascular lesion of anterior spinal or paramedian branches of the vertebral arteries leading to infarction in the medial medulla – affecting the pathways and nucleus mentioned as 4 “M”.
Clinical features of Medial medullary (Djerine’s) Syndrome:
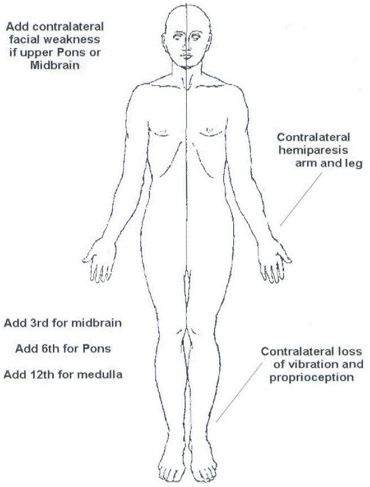
- Motor pathway dysfunction: Contralateral upper motor neuron paralysis on body except face
- Medial lemniscus dysfunction: Contralateral loss of discriminative touch, vibratory and position sense on body except face
- Medial longituidnal fasciculus: Ipsilateral internuclear ophthalmoplegia (failure of adduction of ipsilateral eye towards nose i.e. CN III function and nystagmus in the opposite eye as it looks laterally i.e. CN VI) – this is because CN VI of the opposite eye sends fibers to opposite medial longitudinal fasciculus (MLF) through which fiber goes to CN III
- Motor nucleus of hypoglossal nerve (CN XII): Ipsilateral paralysis of tongue with tongue deviation on protrusion towards affected side