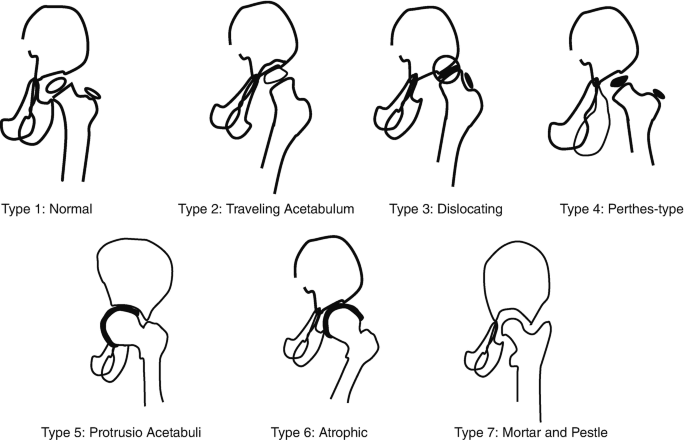
Classification
| Stage/ Type | Pott’s spine (Kumar’s) | Pott’s paraplegia (Tuli) | Hip and Knee | Hip (Shanmugasundaram) |
| I | Predestructive (Straightening, spasm, hyperemia) | Negligible (Objective plantar extensor response or ankle clonus) | Synovitis (ROM 75-100%/Haziness, rarefaction) – Hip: FAbER, Apparent lengthening | Normal (C) |
| II | Early destructive (Diminished space, paradiscal erosion, K<10) | Mild (Subjective neuro-deficit but walks with support) | Early arthritis (ROM 50-75%/+Erosions) – Hip: FAdIR, Apparent shortening | Travelling/Wandering acetabulum (C,A) |
| III | Mild kyphosis (2-3 veretbrae, K 10-30) | Moderate (Paralysis in extension, sensory deficit <50%) | Advanced arthritis (ROM <25%/reduction of joint space) – Hip: FAdIR, True shortening | Dislocating (C) |
| IV | Moderate kyphosis (>3 veretbrae, K 30-60) | Severe (III + Paralysis in flexion, sensory deficit >50%/sphincters involved) | Subluxation/dislocation, ROM <25% – Hip: Wandering acetabulum – Knee: Triple deformity | Perthes (C) |
| V | Severe kyphosis (>3 vertebrae, K >60) | Seddon’s classification: | Aftermath (deformity and ankylosis) – FAbER deformity can occur in hip instead of FAdIR due to continued posture for pain relief or destruction of iliofemoral ligament | Protrusio acetabuli (C,A) |
| VI | Group A (Early onset): within 2 years of active disease | Atrophic (A) | ||
| VII | Group B (Late onset): after 2 years | Mortar and pestle (C,A) |
Seddon’s Group A Pathology: Inflammatory edema, granulation tissue, abscess, caseous material or cord ischemia
Seddon’s Group B Pathology: Recrudescence of disease or mechanical pressure on cord (sequestra, debris, internal gibbus or canal stenosis)
Management
Conservative management
1. Admission: Indications –
- Complications
- Requiring traction to correct deformities under supervision
2. Anti-tubercular therapy:
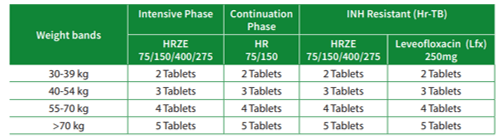
a. National Tuberculosis Management Guidelines, 2019 (Nepal):1
- Musculoskeletal TB: 2HRZE + 7HRE
- Retreatment cases: Drug susceptibility test performed (Genxpert MTB/RIF)
- Rifampicin resistant: Send to DR center for treatment
- Rifampicin sensitive: Isoniazid sensitivity test (Line probe assay/LPA)
- Isoniazid resistant: 6(H)RZE-Lfx
- Isoniazid sensitive: 2HRZE + 4HR
- LPA test unavailable (Isoniazid unknown): 6HRZE
b. Nepal Orthopedic Association Regimen, 2005:2
- Pott’s spine: 18 HRE and 3Z
- Osteoarticular TB: 12 HRE and 3Z
- Soft tissue TB: 9HRE and 3Z
Numbers designate ‘months’ of therapy required; Intensive phase + Maintenance phase; H = Isoniazid; R = Rifampicin; Z = Pyrazinamide; E = Ethambutol
3. Activity limitation (Bed rest), Application of traction (Traction), Active and Assisted motion and Ambulation:
Bed rest: Hard bed (to prevent kyphosis progression in early stage in Pott’s spine)
Functions of traction:
- To correct a deformity
- To maintain the limb in the position of ease during early active stage
- Hip: FAbER
- Knee (use double traction): Flexion
- To offer unhindered observation regarding the local response to treatment
- To hold the inflamed joint surfaces apart
- To permit repetitive guarded assisted and active joint motion
Active and assisted motion of joint on traction (5-10 min/hr): Repetitive motion encourages mesenchymal reparative cells to differentiate into:
- Health synovial membrane
- Well-lubricated useful fibrocartilage adapted to the function of joint
Ambulation: Remember rule of “3”
- Ambulation started after 3weeks – 3 months in spine and 3 months in hip and knee
- Non-weight bearing for initial 3 months in hip and knee
- Partial and Protected weight bearing for next 3 months in hip and knee
- Unprotected weight bearing (crutches and orthosis) discarded after:
- 6-12 months in cases of hip and knee
- 18-24 months in case of Pott’s spine
Thomas test of recovery: During ambulation phase, if symptoms or signs increase, the patient goes back a stage and if there is steady progress, he/she goes forward.
4. Abscess, Effusion and Sinuses:
- Palpable abscesses and large joint effusions: Aspiration + Instillation of 1 gm streptomycin +/- isoniazid
- Drainage indications:
- Failed aspiration or too thick pus
- Prevertebral abscess: in cervical region complicated by difficulty in swallowing and breathing
- Paravertebral abscess: radiological size increases markedly in-spite of treatment
- Sinus tract doesn’t heal within 6-12 weeks under ATT: Excision of tract
5. Anticipated and Accepted Ankylosis in Advanced arthritis:
a. 1st 6 months: Immobilization in functional position
- Hip: 10-30 degrees (1 degree per year of age upto 30 years; younger the spine, more mobile and adaptable it is to compensate for loss of movements at the hip joint) flexion based on age (for ground clearance during walking and comfortable sitting position); 0-5 degrees adduction and 0-15 degrees external rotation
- Knee: 5-10 degrees flexion (for ground clearance during walking)
b. Next 6 months: Partial weight bearing on plaster
c. Next 12 months: Protected weight bearing on crutches and orthosis
6. Analyze:
- X-ray and ESR: 3-6 month interval
- MRI and CT: 6 months interval for 2 years
Surgical management in Hip and Knee
Stage I (Non-responsive): Arthrotomy and synovectomy
Stage II (Non-responsive): Above + Debridement (loose bodies, debris, pannus, loose articular cartilage, osseous juxta-articular foci)
Stage III and IV (Unacceptable position or non-functional ROM or painful fibrous ankylosis):
- Arthrodesis after acceptability test (immobilize in plaster cast and send home for 3-6 weeks):
- Knee:
- Charnley’s compression clamps
- Replace 1 Unit blood postoperatively (expected loss from raw cancellous bone ends)
- 1st 6 weeks: Frequent tightening of screws, initially by 1 round and later by 1/2 to 1/3 of the round every 24 hours
- Next 6 weeks to 6 months: Weight bearing in plaster cast
- After sound fusion in X-rays: Unprotected weight bearing
- Hip:
- Painful fibrous ankylosis/Active disease/Biopsy needed: Intra-articular arthrodesis
- Remove Steinmann’s pin after 6-8 weeks and apply single hip spica
- Weight bearing in hip spica (for 4-6 months) until radiological evidence of bone fusion then remove hip spica
- Protected weight bearing in crutches for next 12 months
- Other options:
- Adduction deformity: Ischio-femoral arthrodesis (extra-articular)
- Abduction deformity: Ilio-femoral arthrodesis (extra-articular)
- Painful fibrous ankylosis/Active disease/Biopsy needed: Intra-articular arthrodesis
- Knee:
- Excision arthroplasty (hip):
- Excision of femoral head, neck, proximal part of trochanter and acetabular rim
- 1st 3 months: Postoperative upper tibial skeletal traction in 30-50 degrees abduction to distract the joint and make favorable environment for pseudoarthrosis (encourage sitting and active assisted movements)
- Next 3-6 months: Crutch walking
- Finally: Walking stick in contralateral hand
- Complications: Shortening (mean 1.5 cm), Instability, Telescoping, External rotation deformity
- Pelvic stabilization operations can be done concurrently or after 3-6 months:
- Pelvic support osteotomy at level of ischial tuberosity: Milch-Bachelor type
- Shelf osteotomy of acetabulum
- Combined
- Pelvic stabilization operations can be done concurrently or after 3-6 months:
- Replacement arthroplasty in active stage (controversial): Atleast 2-3 months of ATT preoperatively
Stage V: Unacceptable deformity or non-functional ROM
- Painless ankylosis in unacceptable position (children and adult): Extra-articular corrective osteotomy
- Hip: Trochanteric osteotomy
- Knee: Supracondylar osteotomy
- Children:
- Fibrous ankylosis without gross distortion of joint anatomy: Subtotal excision of contracted fibrous capsule (arthrolysis)
- Adult:
- Painful ankylosis: Arthrodesis
- Arthroplasty (replacement):
- Minimum disease free period: 1-3 years
- Postoperative ATT: for 5 months
Surgical management in Spine
1. Decompression (+/- fusion): Pott’s paraplegia
- Failure to respond to 3-6 weeks of conservative therapy
- Tuli grade IV Pott’s paraplegia (advanced)
- Anterolateral vs Posterolateral approach:
- AL approach:
- Constrotransversectomy: 2-4 ribs about 8 cm from transverse process + Transverse process
- Debridement: Removal of liquid pus, caseous material, sequestra, necrotic debris
- Pedicle removal: 2-4 pedicles, traced medially using intercostal nerve (which is cut 6 cm lateral to intervertebral foramina)
- Vertebrectomy: All offending diseased bodies and discs are removed
- Outcome: Cord comes to lie in the free place anteriorly
- PL approach: Dura is exposed by hemilaminectomy 1st and then extended laterally to remove the posterior ends of 2-4 ribs, corresponding to transverse process and pedicles
- AL approach:
| Anterolateral decompression | Posterolateral decompression | |
| Advantages | Pathology lies anteriorly | Better fixation and good correction of kyphotic deformity |
| Disadvantages | Osteoporosis due to infection – poor anchorage of instrumentation |
2. Debridement (+/- fusion): Pott’s spine
- Failure to respond to 3-6 months of non-operative treatment (persistent active disease)
- Young children with extensive dorsal lesions (to prevent severe kyphosis)
3. Debridement +/- Decompression +/- Fusion:
- Recurrence of disease or of neural complication
- Approaches:
- C1-C7/T1: Anterior
- T2-T12/L1: Anterolateral or Transpleural (rare)
- L1-L5/S1: Retroperitoneal or Retro-psoas transverse vertebrectomy
4. Fusion (Posterior spinal arthrodesis):
- Symptomatic mechanical instability in healed disease
5. Anterolateral transposition of cord through extrapleural anterolateral approach:
- Neural complications due to severe kyphosis (mandatory if K >60 i.e. Kumar’s grade V Pott’s spine)
6. Laminectomy: Only in –
- Spinal tumor syndrome (extradural granuloma/tuberculoma)
- Secondary vertebral canal stenosis without much deformity (healed disease)
- Non-healing posterior spinal disease
Complications of Spine Surgery
- Bleeding from paravertebral venous plexus and from the vessels in dense fibrous tissues
- Excessive fall of blood pressure (lag of adrenal cortex): Preoperative or intraoperative steroids may help
- Tear of pleura (adhesions)
- Tear of dura:
- Close by continuous non-absorbable sutures
- Small and/or not possible to close: Seal with a small piece of gelfoam/sponiostan or muscle
- Do not use postoperative suction drain
- Recumbent position for 48-72 hours in postoperative period (helps to prevent CSF leak and help sealing the tear)
Stages of healing of disease:
- Invasion and destruction (at onset)
- Control and regression
- Healed stage:
- Disappearance of all systemic features of activity
- Disappearance of local warmth, tenderness, spasm, abscess, sinuses
- Return of painless motion (in early disease)
- Normal or non-progressive ESR
- X-ray: Remineralization and restoration of bony outlines and trabeculae and sharpening of cortical and articular margins
- MRI: Resolution of edema of soft tissues and bones, and soft tissue collection; reconstitution of destroyed areas of bone
- Paradiscal spine TB without surgery:
- 70%: osseous replacement
- 20%: fibrous replacement
- 10%: fibro-osseous replacement
- Paradiscal spine TB with surgery:
- 90%: osseous replacement
- 10%: fibro-osseous replacement
- Paradiscal spine TB without surgery:
Neural recovery after Surgery
- First evidence of objective recovery: within 3 weeks
- Near complete recovery: 3-6 months
- No recovery: after 12-28 months
- Persistence of extensor plantar response at 18 months: 55% patients
- Early return of flexor response in cases of milder neurological involvement of shorter duration
- Recurrence and relapse possible
Course of Kyphosis in Non-operated Cases
- Destruction of thoracic vertebral body results in a posterior displacement of the center of motion, a subluxation at the level of articular facets and increase in the weight to be borne by the anterior part of the body
- In the lumbar spine, the large bodies and vertical orientation of articular facets are more apt to telescope than to angulate
- Ther cervical spine was prevented from telescoping by the interposition of transverse processes
- Incidence of kyphosis is more common in thoracic spine:
- Gravity perpetuates pre-existing kyphotic curve
- Once K> 30 degrees, vertical forces are converted into translational forces
- Once K >45 degrees, posterior spinal muscles are put to a mechanical disadvantage further adding to deformity
- Takes place during active spinal growth with or without active disease (unrestricted growth of posterior elements in presence of restricted growth of vertebral bodies)
- Upper dorsal spine: Some degree of protection by the rib cage
- Below D9: Worst prognosis (absence of complete ribs)
- Posterior subluxation due to horizontal orientation of posterior articular facets:
- Phase I (active disease): Anterior column collapse
- Phase II (healed disease): Arrest of growth potential of vertebral bodies
Course of Kyphosis in Surgical Patients
- Future angle of kyphotic deformity (Y) = 5.5 + 30.5 X Pre-treatment vertebral loss
- Only operative procedure that has been claimed to prevent increase of kyphotic deformity is the Hongkong procedure (radical anterior debridement + vertebral body removal + strut grafting)
Reference: Tuberculosis of the Skeletal System: Bones, Joints, Spine, and Bursal Sheaths – S. M. Tuli, 6th Edition

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.