Follow-up protocol Post-Evacuation of Molar Pregnancy
- Weekly hCG measurements until hCG becomes undetectable
- Once hCG is undetectable, 2 further specimens should be obtained at weekly intervals
- Then monthly for 6 months and then
- Every 2 months for a further 6 months 1
Diagnosis of GTN
The diagnosis of GTN is made on the basis of elevated hCG levels supported, if possible, by histologic or radiologic evidence. The agreed criteria to diagnose GTN include:
1. At least 4 values of persistently elevated hCG plateau (days 1, 7, 14, and 21) or longer, or
2. Sequential rise of hCG for 2 weeks (days 1, 7, 14) or longer. The actual values of hCG are left to the discretion of individual physicians.
3. Lung metastases are diagnosed by chest X-ray
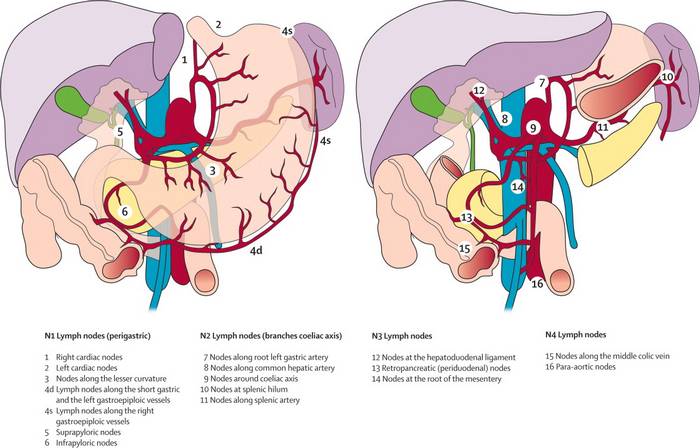
FIGO Anatomic Staging of GTN
Stage I – Confined to uterus
Stage II – Outside uterus but within genital tracts
Stage III – Lung metastases
Stage IV – All other metastases
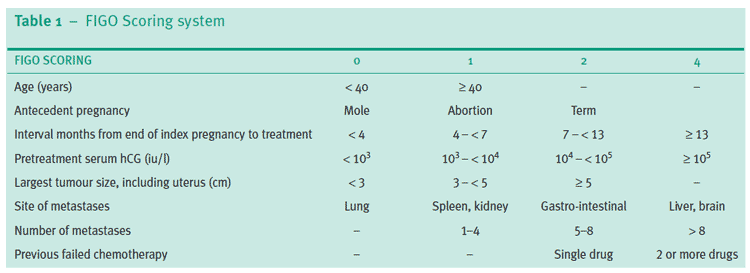
WHO Prognostic Score for GTN
Management of GTN
| Low risk GTN | High risk GTN | |
| Definition | WHO Score ≤6 in FIGO Stage I-III | WHO Score >6 in FIGO Stage I-III or FIGO Stage IV |
| Management | Initiate single agent methotrexate or dactinomycin regimen
|
Evaluate for high risk metastase: brain, liver, kidney |
| Consider hysterectomy if fertility not desired | Stabilize medical status of patient. | |
| Monitor hematologic, renal, and hepatic indices before each cycle of chemotherapy | Multi-agent therapy with EMA/CO or MAC
EMA/CO regimen:
If resistant: EMA-EP regimen |
|
| Change to alternative single agent if resistance or severe toxicity to 1st agent | Management of liver metastases: Consider selective angiographic embolization or irradiation | |
| If resistance to alternative agent:
1. Repeat metastatic evaluation 2. Consider hysterectomy is no extrauterine metastases 3. Multiagent chemotherapy (MAC or EMA/CO) |
Management of brain metastases:
1. Consider early neurosurgical intervention if isolated brain lesion. 2. Consider stereotactic or whole brain irradiation if multiple brain lesions. |
|
| Remission: 3 consecutive weekly hCG values in the normal range. | Monitor hCG weekly during therapy. | |
| 1 or 2 cycles of maintenance/consolidation therapy | Atleast 3 cycles of maintenance chemotherapy after hCG values normalize. |
E – Etoposide; M – Methotrexate; A – Actinomcyin D; C – Cyclophosphamide; O – Oncovin (Vincristine); P – Platinum
Surveillance during and After Therapy for GTN
1. Monitor serum quantitative hCG levels every week during chemotherapy:
a. Response: >10% decline in hCG during 1 cycle
b. Plateau: +/- 10% change in hCG during 1 cycle
c. Resistance: >10% rise in hCG during 1 cycle or plateau for 2 cycles of chemotherapy
- Evaluate for new metastases
- Consider alternative chemotherapy
- Consider extirpation of drug-resistant sites of disease
2. Remission: 3 consecutive normal weekly hCG
- Maintenance chemotherapy
3. Surveillance of remission:
- hCG values 2 weekly X 3 months
- hCG values monthly to complete 1 year of follow-up
- hCG vaules every 6-12 months indefinitely; atleast 3-5 years.
Placental Site Trophoblastic Tumor (PSTT)
- Origin: Intermediate trophoblast at the site of placental attachment.
- Serum marker: Free beta-hCG (high hCG-H in choriocarcinoma)
- Immunohistochemical marker: human placental lactogen (hPL)
- Treatment:
- Non-metastatic: Hysterectomy
- Metastatic: Chemotherapy EMA-EP regimen (Alternative: TE/TP regimen where T stands for Taxol)
Pregnancy after Chemotherapy
It is recommended to delay pregnancy until 12 months (1 year) after completion of chemotherapy for 2 main reasons:
- Minimize any possible damaging effects on developing oocytes.
- Minimize the confusion over disease relapse from the hCG produced during pregnancy.