Introduction:
- Is a tumor of mesenchymal origin (previously thought to be of smooth muscle origin)
- Most common mesenchymal neoplasm of GI tract
- Arise from interstitial cells of Cajal
- Incidence: 7-15 cases per million per year
- 95% overexpress KIT (CD117), 80% express BCL-2 and 70% express CD34
- KIT negative GIST will express PDGFRA
- Sites: stomach (40-60%), SI (20-40%), colon/rectum (5-15%)
Other facts:
- Gastric GIST arise most commonly after 50 years
- 5% of all GIST are associated with an underlying heritable mutation such as familial GIST syndrome (mutation in KIT and PDGFRA), NF-1, Carney-Stratakis syndrome (GIST+paraganglioma+/-pulmonary chondroma)
- 2 pathological variants: spindle cell (70%)> epithelioid (30%)
Clinical features:
- Non-specific symptoms: early satiety, bloating and vague abdominal pain
- Bleeding: Malena or frank hematemesis
- Tumor rupture with intra-abdominal hemorrhage is uncommon, but when it occurs, it requires urgent surgical intervention.
Diagnosis:
- CECT with IV and oral contrast is the IOC: helps in diagnosis as well as staging of disease and is non-invasive
- MRI is indicated only when there is contraindication of CT and for rectal GIST.
- Staging of the disease is important especially when the patient is considered for neoadjuvant imatinib therapy.
- PET-CT is the gold standard investigation for recurrent GIST.
Role of biopsy/tissue diagnosis in GIST (current consensus):
- Is not recommended as it is a submucosal tumor (go for direct upfront surgery if there is high suspicion of GIST in imaging and the disease is operable)
- If there is diagnostic dilemma then go for biopsy
- EUS guided FNA is superior to UGI endoscopy guided biopsy as the tumor is submucosal.
- Sensitivity and specificity of EUS guided FNA: 82% and 100% respectively
Treatment:
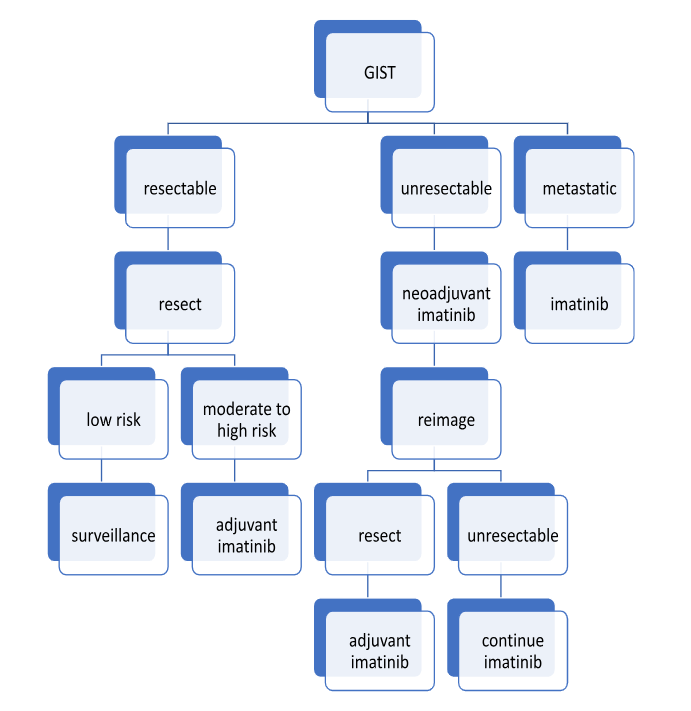
- Mainstay of treatment: complete surgical excision
- Indication of surgery: size >2 cm and symptoms
- For tumors <2 cm:
- If high risk features are present on endoscopy or EUS go for surgery
- If not can be observed with 6-12 monthly EUS/endoscopy follow up
High risk features:
- Irregular borders
- Ulceration
- Echogenic foci
- Heterogeneity
Choices of surgery:
- Depending on tumor size and sites surgeries can vary from wide local excision, enucleation, sleeve gastrectomy, or total gastrectomy.
Aim of surgery:
- R0 resection
- Lymph node dissection is not required as lymphatic metastasis is very rare
- Tumor should be handled carefully intraoperatively to avoid rupture or spillage.
Prognostication:
- 2 main prognostic factors:
- Tumor size
- Mitotic rate
- Based on long term follow up study of 1700 patients with Gastric GIST, malignant potential based on combination of these 2 factors have been established as shown below:
| Malignant potential | Comments | Mortality |
| Benign | Size: up to 2 cmMitosis: up to 5/50 hpf | No tumor related mortality |
| Probably benign | Size: 2-5 cmMitosis: same as above | <3% |
| Uncertain/ low malignant potential | Size: up to 2 cmMitosis: >5/50 hpf | – |
| Low to moderate | Size: >10 cm Mitosis: same as benignORSize: 2-5 cmMitosis: >5/50 hpf | 12-15% |
| High | Size: 5-10 cm Mitosis: >5/50 hpfORSize: >10 cmMitosis: >5/50 hpf | 49-86% |
Role of adjuvant therapy:
- Drug of choice: imatinib (tyrosine kinase inhibitor)
- Indication: metastatic disease, resectable but moderate to high-risk malignant potential
- Can be used as neoadjuvant therapy if the disease is non-metastatic but unresectable.
Landmark trials in GIST:
- ACOSOG Z9001 trial:
- C-KIT positive tumors 3 cm or larger who underwent complete resection found that patients treated with imatinib for 1 year had significantly improved 1 year recurrence free survival (98% VS 83%).
- Scandinavian Sarcoma group trial:
- Compared adjuvant course of imatinib (36 months VS 12 months) after resection of high-risk GIST
- Result: extended course (36 months) had higher 5-year RFS and OS.
- This trial has established a 3-year course as the standard of care after resection of high-risk GIST.
Algorithm for management of GIST:
Reference: Sabiston textbook of surgery 21st edition

He is an avid reader, guitar player, melodious singer and old songs lover. He has a passion for making medical knowledge accessible and comprehensive.