Etiology and Risk factors of Gastric Carcinoma
Mnemonic: 14 “A”s
- Animal foods (smoked, cured or preserved – contains high nitroso- compounds)
- Anti-oxidant poor foods
- Acetaldehyde in Alcohol
- Acid peptic disease or Antigen i.e. H.pylori
- Atrophic gastritis and Achlorhydria
- Adenomatous polyps (precursor of intestinal type of gastric cancer)
- A type Blood group
- Asians (Japan) and African-Americans
- Antral resection (Partial gastrectomy)
- Age >60 years
- Alkaline bile reflux (in stump carcinoma)
- Ancestral (Hereditary diffuse gastric cancer, Hereditary breast/ovarian cancer, Lynch syndrome, Li-fraumeni syndrome, FAP, etc.)
- Acquired hypogammaglobulinemia (Common variable immunodeficiency or CVID)
- Albumin (protein) losing enteropathy with hypertrophy of gastric mucosa (Menetrier’s disease)
Symptoms and Signs of Gastric Carcinoma
Mnemonic: 11 “A”s
- Asymptomatic (often in Early Gastric Carcinoma)
- Abdominal pain or discomfort i.e. epigastric (commonest early symptom)
- Classic triad: Anemia (including GI bleeding), Anorexia and Asthenia (weight loss is the commonest symptom)
- Aphagia (Dysphagia): cancer of proximal stomach i.e. GE junction or cardia
- Abdominal mass i.e. epigastric (advanced disease)
- Adenopathy
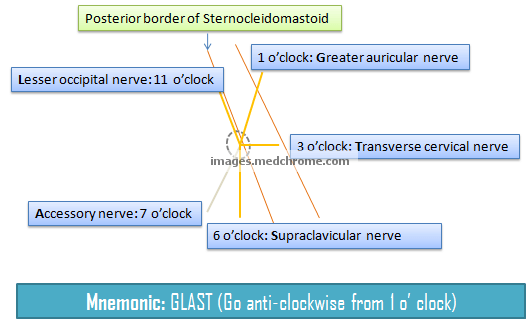
- Virchow’s node: left supraclavicular node (Troisier sign)
- Irish node: left axillary node
- Advanced signs in Abdominal cavity:
- Ascites and hepatomegaly
- Blumer’s shelf (palpable nodule in pouch of douglas – peritoneal carcinomatosis; indicates dissemination)
- Sister Mary Joseph nodule (palpable nodule in umbilicus – peritoneal carcinomatosis; indicates dissemintation)
- Adjacent organ metastases: Krukenberg’s tumor (mucin-producing signet-ring cells in ovaries)
- Acanthosis nigricans (Paraneoplastic syndrome)
WHO Histologic Classification
a. Adenocarcinoma (90%)
Lauren type – Intestinal
- Tubular (commonest)
- Papillary
- Mucinous
Lauren type – Diffuse
- Signet-ring cell carcinoma
In contrast to intestinal type of gastric carcinoma, diffuse type of gastric carcinoma are more common in younger patients, females, have more propensity for peritoneal dissemination and carry worse prognosis.
b. Uncommon variants: Adenosquamous carcinoma, Squamous carcinoma, Lymphoma, Carcinoids
Gross Morphologic Classification
Most common site: Antrum – lesser curvature side
Early Gastric Cancer (EGC)
Limited to mucosa and submucosa (lymph nodes may or may not be involved)
3 types based on Endoscopic appearance:
- Type I – Protruding
- Type II – Superficial (a – elevated; b – flat; c – depressed)
- Type III – Excavating
Type IIc is the most common Early Gastric Cancer.
Advanced Gastric Cancer
Invades gastric wall beyond submucosa
5 types based on Borrmann’s classification:
- Type I – Polypoid or fungating carcinoma (25% of advanced gastric carcinoma)
- Type II – Ulceroproliferative (36% of all gastric carcinoma)
- Type III – Ulcerative (25% of advanced gastric carcinoma)
- Type IV – Diffusely infiltrating carcinoma (linitis plastica)
- Type V – Unclassified
Reliable Serologic Marker
CA 72-4
Spread of Gastric Carcinoma
Direct spread:
- Into the layers of stomach wall
- Into pancreas, colon, liver and diaphragm
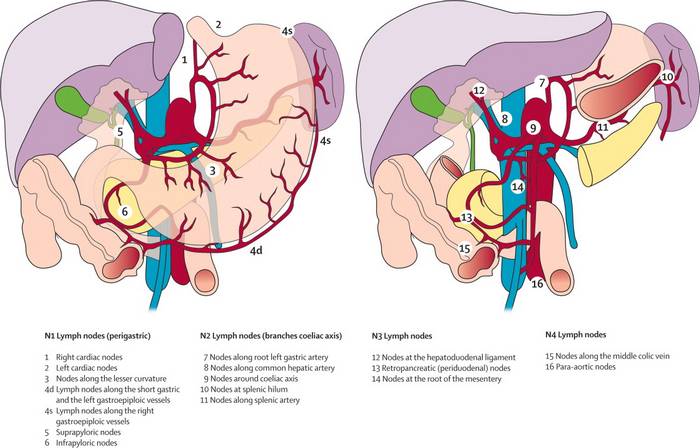
Lymphatic spread:
- Troisier’s sign: invovlement of left supraclavicular node
Hematogenous spread:
- First to liver
- Uncommon in the absence of nodal metastasis
Transperitoneal spread:
- Ascites
- Blumer’s shelf (deposits in the rectovesical pouch)
- Sister Joseph’s nodule (deposits around the umbilicus)
- Krukenberg tumor (deposits over the ovary, typically bilateral, cut-section shows normal ovary with surface deposits)
Simplified TNM and Staging of Gastric carcinoma
Signs of Inoperability
- Hematogenous metastasis
- Involvement of distant peritoneum
- Ascites
- Fixation to nonremovable adjacent structure (pancreas, diaphragm)
- N4 nodes
Treatment
Operable tumors
- Antral growth: Subtotal gastrectomy with reconstruction procedure (Billroth I or II or polya)
- Body, fundus growth: Total gastrectomy with reconstruction procedure (Jejunal interposition or Roux-en-Y loop)
Reconstruction procedures:
- Billroth I: Gastroduodenal anastomosis (kocherization – mobilization of 1st part of duodenum)
- Billroth II: Gastrojejunal anastomosis (anterior to transverse colon) with closure of proximal stump
- Since, calcium in diet is absorbed in 1st part of duodenum which is bypassed in gastrojejunal anastomosis, hypocalcemia is a potential complication.
- Duodenal stump blow out: most common on 4th day; no need to intervene immediately, can be treated with USG guided drainage
- Polya: End to side anastomosis
- Jejunal interposition: Esophagojejuno-duodenal anastomosis; risk of Hunt-Larence pouch formation (jejunum folded on itself to form pouch)
- Roux-en-Y loop:
- Y loop: afferent loop should be small
- Roux loop: should be 40-60 cm to avoid bile reflux
Inoperable tumors (Palliative procedures)
1. Pylorus end:
- Tanner’s anterior gastrojejunostomy
- Devine’s exclusion bypass
2. Cardia end:
- Stent
- Laser luminization
- Souttar’s tube
3. Ultimately inoperable:
- Linitis plastica – feeding jejunostomy
Distant metastases
Chemotherapy only:
- FAM therapy:
- 5-Fluorouracil
- Adriamycin
- Mitomycin C
- ECF regimen (Cunningham’s royal marsden regimen)
- Epirubicin
- Cisplatin
- 5-Fluorouracin

excellent summary for quick revision.keep it up