Definition: Symptomatic inflammation of the lining mucosa of nose and paranasal sinuses. Uncomplicated rhinosinusitis is defined as rhinosinusitis without clinically evident extension of inflammation outside the paranasal sinuses and nasal cavity at the time of diagnosis (eg, no neurologic, ophthalmologic, or soft tissue involvement).
Types: Based on duration
- Acute Rhinosinusitis (ARS): < 4 weeks
- Subacute Rhinosinusitis: 4-12 weeks
- Chronic Rhinosinusitis: > 12 weeks
- Reccurent Rhinosinusitis: ≥ 4 episodes per year without persistent symptoms in between
Causes of Acute Rhinosinusitis:
- Rhinogenic (spread of rhinitis): commonest
- Dentogenic: Dental root infection, Apical granuloma, Maxillary sinus fistula
- Traumatic: Road traffic accident, Barotrauma, Nasal picking, Septal surgery
- Diving and swimming
- Hematogenous: Rare
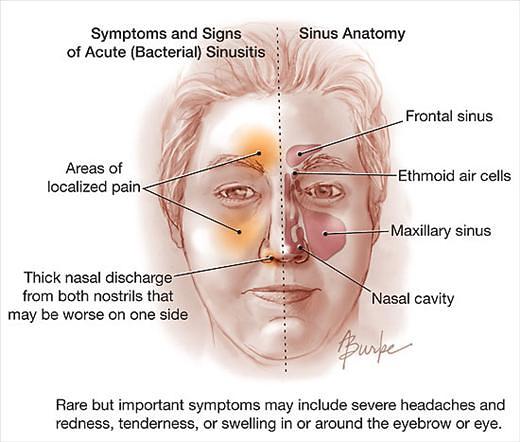
Sinus Involvement in Acute Rhinosinusitis:
- Children: Ethmoid sinus (Due to inadequate pneumatization of other sinuses)
- Adults: Maxillary sinus, ethmoid cells, frontal sinus, and sphenoid sinus in descending order
Causative organisms of Acute Rhinosinusitis:
- Viral: (most common) rhinovirus, parainfluenza virus, respiratory syncytial virus, influenza virus, coronavirus
- Bacterial: S. pneumoniae (most common bacteria), H. influenzae, M. catarrhalis, S. aureus, S. pyogenes
- Fulminant Fungal: Aspergillus, phaeohyphomycosis, Mucor, Rhizopus
Clinical Guidelines for Acute Rhinosinusitis (ARS):
- Diagnose Acute Rhinosinusitis (ARS): Up to 4 weeks of purulent nasal drainage (anterior, posterior, or both) accompanied by nasal obstruction, facial pain-pressure-fullness, or both.
- Additional features: fever, cough, fatigue (malaise), reduced sense of smell (hyposomia), lack of the sense of smell (anosmia), maxillary dental pain, and ear fullness or pressure
- Differential diagnosis: Distinguish between Bacterial and Viral cause
- Viral (VRS): symptoms or signs of acute rhinosinusitis are present less than 10 days and the symptoms are not worsening
- Bacterial (ABRS): symptoms or signs of acute rhinosinusitis fail to improve within 10 days or more beyond the onset of upper respiratory symptoms, or symptoms or signs of acute rhinosinusitis worsen within 10 days after an initial improvement (double worsening)
- Radiographic imaging: With-hold radiographic imaging for patients who meet diagnostic criteria for ARS, unless a complication or alternative diagnosis is suspected
- Sinus involvement is common in documented viral URIs, making it impossible to distinguish ABRS from VRS based solely on imaging studies
- Initial diagnostic evaluation:
- Measurement of vital signs
- Physical examination of head and neck:
- Hyponasal voice (Nasal obstruction)
- Swelling or erythema over involved cheek bones or periorbital area
- Palpable cheek tenderness or percussion tenderness of the upper teeth
- Purulent drainage in the nose or posterior pharynx
- Signs of extra-sinus involvement (orbital or facial cellulitis, orbital protrusion, abnormalities of eye movement, neck stiffness)
- Culture of nasal or nasopharyngeal secretions: correlate poorly with maxillary sinus culture
- Symptomatic relief of Acute Rhinosinusitis (ARS):
- Analgesics: for pain and fever
- Nasal saline irrigation (preferably hypertonic saline)
- Topical intranasal steroids: Only 1 out of 15 benefit from it
- Decongesants: for obstruction (but avoid use beyond 3 days to prevent rhinitis medicamentosa)
- Initial management of Acute Bacterial Rhinosinusitis (ABRS):
- Watchful waiting (without antibiotics): Only when followup is assured OR
- Antibiotic therapy:
- Amoxicillin with or without clavulanate as first-line therapy for 5 to 10 days
- For penicillin-allergic patients: Doxycycline or a respiratory fluoroquinolone (levofloxacin or moxifloxacin)
- For Non-type I hypersensitivity to penicillin: Clindamycin plus a third-generation oral cephalosporin (cefixime or cefpodoxime)
- Treatment failure for ABRS: failure to improve with initial management by 7 days or worsening of symptoms
- If on watchful waiting: Start antibiotics
- If on antibiotic therapy: Change antibiotics
Recently, the Task force criteria for diagnosis of ARS has been eliminated. It used the combination of major and minor criteria. The major criteria included: facial pain/pressure, nasal obstruction, nasal discharge or discolored postnasal drip, hyposmia/anosmia, purulence on examination and fever. The minor criteria included: headache, halitosis, fatigue, dental pain, cough and ear pain/pressure/fullness. Diagnosis was made if 2 major OR 1 major + 2 minor criteria were fulfilled.