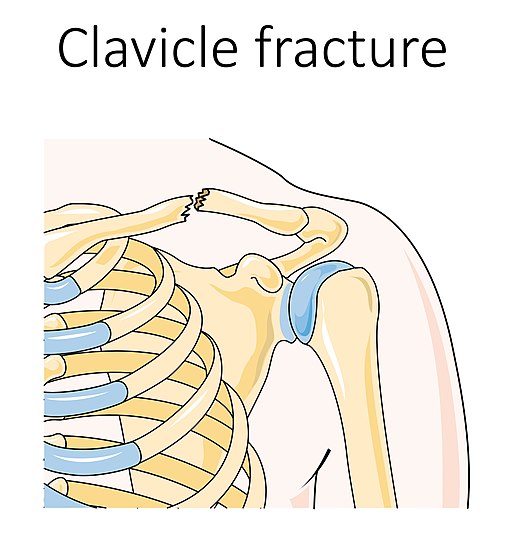
1. 80-85% are mid-shaft fractures (other 10-15% are lateral 3rd and 5% are medial 3rd fractures) because of:
- Narrow cross-section
- Scarce muscle attachment
2. Deforming forces:
- Medial (proximal) fragment: pulled postero-superiorly and into external rotation by sternocleidomastoid (can stretch the overlying skin)
- Lateral (distal) fragment: Pulled –
- Inferiorly: by weight of arm and deltoid
- Medially and into internal rotation: by pectoralis major and latissimus dorsi (also causes scapular protraction and prominence of inferior scapular angle as scapula moves along with lateral end of clavicle)
3. X-ray views:
- Standard AP view
- Mid-shaft fracture:
- AP cephalic tilt view (20-30 degrees cephalad tilt; eliminates overlap of thoracic cage)
- Apical oblique view (45 degrees oblique and 20 degrees cephalic tilt; useful in pediatric fractures where significant curvature is present in bone)
- Lateral third fractures and ACJ: Zanca view (15 degrees cephalad tilt with 50% penetration)
- Medial third fractures and SCJ: Serendipity view (40 degrees cephalad tilt)
4. Allman classification:
- Group 1: Middle 1/3
- Group 2: Lateral 1/3 (with Neer’s subdivision) –
- Type I: Lateral to CC ligaments (stable)
- Type IIA (Rockwood): Medial to CC ligaments; unstable (50% non-union; operative management recommended)
- Type IIB (Rockwood): Between CC ligaments; unstable (30-45% non-union, operative management recommended)
- Type III: Intra-articular (stable, but risk of ACJ arthritis)
- Type IV: Physeal
- Type V: Comminuted (operative management recommended)
- Group 3: Medial 1/3 (operative management recommended with posterior displacement)
Dameron and Rockwood classification for lateral 1/3 pediatric fractures:
Type I: Mild strains of ligaments or periosteal tears
Type II: Complete disruption of AC ligaments or lateral periosteal attachment with mild damage to superolateral periosteal sleeve
Type III: Type II + Large disruption of superolateral periosteal sleeve (CC interval >25-100% than normal side)
Type IV: Type III + Posterior displaced (often embedded in trapezius)
Type V: Type III + Superior displaced (occasionally splitting deltoid and trapezisu)
Type VI: Displaced inferiorly (inferior to coracoid)
* Displacement of the distal clavicle through this periosteum in children has been likened to having “a banana being peeled out of its skin.”
5. Non-union rate is 15% in conservative management and 1.5% in surgically treated patients.
6. Operative indications (relative):
- Open fractures and impending open fractures (skin tenting)
- Floating shoulder – with scapular fractures (double disruption of superior shoulder suspensory complex)
- Vascular injury requiring repair
- Brachial plexus palsy
- Displacement >100% or 2 cm (risk of nonunion)
- Shortening or overlap >2 cm (risk of nonunion; associated with poor function outcome and patient dissatisfaction; decreased shoulder strength and edurance)
- Comminuted (>3 fragments; risk of nonunion) and segmental fractures
- High activity level
- Polytrauma
- Patient preference
- Lateral clavicle fracture – Neer type II and V
- Pediatric lateral clavicle fracture – Dameron and Rockwood type IV, V and VI
7. Structures at risk during surgery:
- Superficially on clavicle (run from medial to lateral): 3 branches (anterior, middle, posterior) of supraclavicular nerves (C3,C4) – injury leads to numbness inferior to incision site
- Inferior to clavicle: Subclavian vein, Subclavian artery (more posterior), Brachial plexus (most risky in mid-clavicular fractures; avoid violating subclavicular space) in middle 1/3 and lateral 1/3
- Posterior to clavicle: Subclavian vessels in medial 1/3
8. Recommendations for the optimal treatment of displaced midshaft fractures of clavicle:
- Young active patients will have superior results with primary fixation
- Antero-inferior plating may reduce the risk of symptomatic hardware and breach of sub-clavicular space compared with superior plating
- No difference in outcome between a regular sling and a figure of 8 bandage (if snugged to tightly – can compromise skin and brachial plexus) when non-operative treatment is selected
- No difference in outcome between plating and intramedullary nailing
- Factors associated with poor outcome following non-operative treatment: shortening and increasing fracture comminution
9. Rehabilitation for non-operative treatment:
- Sling/NWB for 6 weeks
- Elbow, wrist and finger ROM initiated immediately
- Passive ROM once discomfort subsides in 7-10 days (ROM in 90 degrees shoulder flexion/abduction avoided for 2-3 weeks to avoid clavicular rotation)
- At 6 weeks, WBAT and full ROM
10. Rehabilitation for operative treatment:
- Immediate postoperative: Sling and gentle pendulum exercises
- 2-6 weeks: Sling discontinued and unrestricted ROM
- 6-12 weeks: Resisted and strengthening exercises if X-rays shows adequate healing
- >12 weeks: Contact and adventurous sports

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.