Mnemonic: BRAIN ATTACK
a. Blood pressure:
Antihypertensives are recommended only in following conditions:
- SBP >220 mmHg, DBP >120 mmHg or MAP >130 mmHg (Target SBP reduction by 15% in 1st 24 hours)
- End organ damage: Acute MI, Aortic dissection, Hypertensive encephalopathy, Severe left ventricular failure
- Candidates for thrombolysis: SBP >185 mmHg and DBP >110 mmHg (Target: SBP ≤185 mm Hg and DBP ≤110 mm Hg)
- For patients with SAH: Prehemorrhage blood pressure or a MAP <140 mm Hg if the baseline blood pressure is unknown.
Drugs and dosing:
If parenteral agents are used, labetalol or nicardipine is favored because of ease of titration and limited effect on cerebral blood vessels. Sublingual nifedipine or sublingual nitroglycerin is not recommended because either agent can produce a precipitous drop in BP.
- Labetalol 10-20 mg IV over 1-2 minutes (may repeat 1 time)
- Nicardipine infusion 5 mg/hr titrated to maximum of 15 mg/hr and when desired BP is reached, reduced to 3 mg/hr
b. Respiration:
- Supplemental oxygen: Only if SaO2 <95% (Target SaO2 >94%)
c. Airway:
- Airway management
- If GCS <9: Intubate
d. Imaging:
- Target door to CT scan completion: 20 minutes
- Target door to CT scan reading: 45 minutes
- Emergent non-contrast CT head:
- To detect Hemorrhages (hyperdense in acute, isodense in subacute) and Stroke mimics
- The ABC/2 technique is a quick and accurate method of measuring ICH volume at the bedside
- Early ischemic changes (within 3 hours): Hyperdense artery sign (acute thrombus in a vessle), sulcal effacement, loss of insular ribbon, loss of grey-white interface, mass effect, acute hypodensity
- Gross signs of infarction (6-12 hours): Hypodensity
- MRI:
- Can visualize ischemic infarcts earlier and identify acute posterior circulation strokes more accurately
- As effective as CT in identifying ICH
e. Normoglycemia:
- Glucose target: 140-180 mg/dl
- If glucose >200 mg/dl: Use sliding scale insulin or GKI
f. Antiplatelets or Aspirin:
- TIA: Aspirin 75 to 325 mg PO daily, Clopidoogrel 75mg PO daily
- Acute ischemic stroke: Aspirin 325 mg within 24 to 48 hours
- 1st 24 hours after rtPA: NO ANTIPLATELETS
g. Temperature:
- Target: 37.0°C±0.5°C (For fareneheit – 32 + celsius X 18)
h. Thrombolysis (rtPA) for ISCHEMIC STROKE:
- Onset to rtPA: within 3 to 4.5 hours
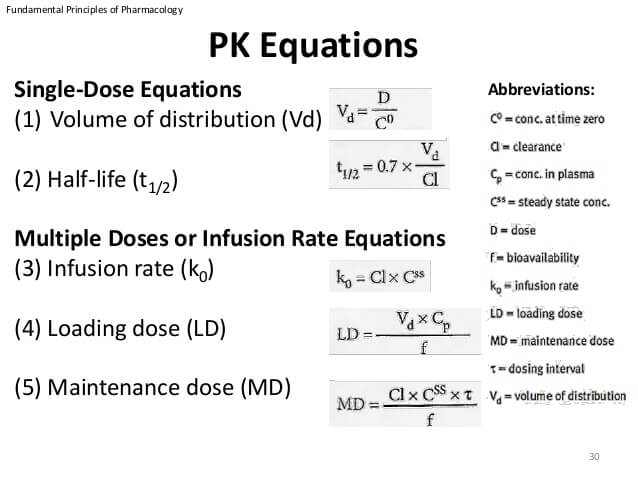
- Dose: 0.9 mg/kg (maximum 90 mg)
- Bolus: 10%
- Remaining: 90% over 60 minutes
- Monitoring: Vital signs and GCS need to be monitored every 15 minutes for two hours using manual BP cuff; every 30 minutes for the next six hours; hourly for the next six hours; and four-hourly for up to two days post-treatment.
- Contraindications:
- <1 week: Lumbar puncture, Arterial puncture, Anticoagulant use
- <2 week: Major surgery or serious trauma
- <3 week: Active internal bleeding (GI or GU hemorrhage)
- <3 month: Intracranial surgery, serious head trauma, previous stroke, MI
- >1/3rd: stroke size >1/3 of cerebral hemispheres
- SBP >185 mmHg and DBP >110 mmHg
- Platelets: <1,00,000/ml
- Glucose: <50 mg/dl or >400 mg/dl
- PT: >15 seconds
- Seizure
- Pregnancy
- Hemorrhage in CT scan
For SAH: Nimodipine 60 mg PO 4 hourly and ICP reduction techniques
i. Assess swallow, nutrition and hydration:
- Perform a bedside swallow screen
- If swallow screen failed (drowsy/unsafe swallow), refer to the speech and language therapist
- If the patient is nil by mouth, prescribe intravenous 0.9% sodium depending on the patient’s state of hydration.
- Avoid dextrose in the first 48 hours unless hypoglycemic
- Consider modified diet or nasogastric feeding at 24 hours and refer the patient to a dietician
j. Continence:
- Indwelling catheters should be avoided post-stroke because of the risk of complications and should only be used when other options have failed
k. Keep uptodate with patient positioning:
- Head-end elevation to 30 degrees (decreases ICP, prevent choking and aspiration)
- Hypoxia inducing positions should be avoided (left sided or slumped in a chair)

Interesting!
Thank you. These mnemonic has been very helpful in remembering the management of stroke patients.