Dated: July 15, 2025
So here we go – not quite Day 1, but definitely the beginning of something new. With two weeks of overlap before the official August 1 start, I reached B&B Hospital at 7:30 AM – early, eager, and quietly absorbing everything around me. As I waited at the reception, I met a few of the other incoming fellows. There was a shared sense of curiosity and quiet anticipation among us, knowing this was the real beginning.
At around 8:15 AM, we were taken to the classroom, where the morning academic ritual was already in motion. The residents were presenting the ER cases admitted overnight. What followed was an intense grilling – rapid-fire questions from attendings, probing every detail. It was clear that this wasn’t just about presenting cases; it was about thinking on your feet and owning every decision.
After that, we were formally welcomed – a moment brief but meaningful. Then we were off to our respective OTs, stepping into the next phase of training. Scrubbed in, eyes wide open, and ears even wider, I felt the shift from observer to participant. The learning had officially begun not just from books or lectures, but from real patients, real decisions, and real pressure.
Case: Left posterior hip dislocation with posterior wall and posterior column acetabular fracture without neruo-vascular dysfunction
Issue: Iatrogenic sciatic nerve palsy following fixation of acetabular fracture
Literature review
Doctors at 2 major trauma centers looked at 922 cases of acetabular fracture surgery done from 2010 to 2020 to see of prone or lateral positioning affected the risk of accidentally injuring the sciatic nerve. They found a much higher risk when patients were prone: about 8.4% of patients in that position experienced nerve palsy, versus only 0.8% in the lateral position. After adjusting for other factors, being prone made nerve injury nearly five times more likely. Greater blood loss during surgery and complex fracture pattern (involving both posterior wall and posterior column) also raised the risk. These 3 risk factors in combination had good ability to predict likelihood of sciatic nerve palsy. Of those who experienced nerve palsy, about 2/3 fully recovered within around 70 days, but 1/3 had lasting weakness. The study concludes that surgeons should strongly consider using the lateral position to reduce nerve injury risk.
Further reading: AM19 Paper 045: Coned Hemipelvis and Total Hip Replacement in Osteoporotic Acetabular Fractures of the Elderly
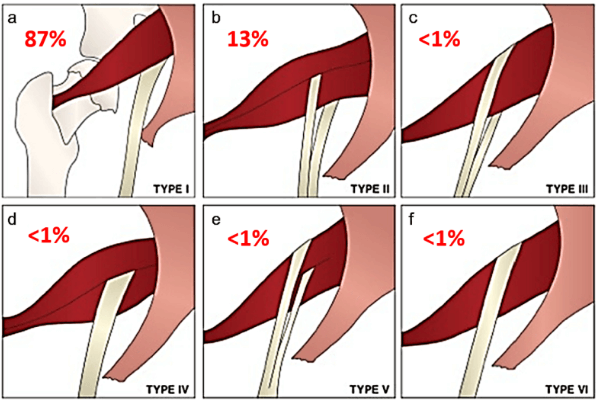
A retrospective review of 644 adult patients who underwent surgical fixation of acetabular fractures via the Kocher-Langenbeck (KL) approach between 2010 and 2022 evaluated risk factors for postoperative sciatic nerve palsy. The overall incidence of nerve injury was 3.1%, with no significant difference observed between lateral and prone positioning. However, transverse fracture patterns were associated with a threefold increase in risk, and individual surgeon variability significantly influenced outcomes. These findings suggest that patient positioning may be less critical than previously thought, while fracture morphology and surgical technique play a more decisive role in sciatic nerve injury risk.
Further reading: Iatrogenic Sciatic Nerve Injury in Posterior Acetabular Surgery: Surgeon More Predictive Than Position – PubMed
A retrospective review of 129 operatively treated acetabular fractures managed via posterior or extensile approaches (including 65 Kocher–Langenbeck procedures) at a Level‑I trauma center between January 1991 and March 1995 found that, without intraoperative somatosensory evoked potential monitoring (SSEP), only one patient sustained an iatrogenic sciatic nerve sensory deficit, and no pre-existing nerve injuries were worsened. The authors concluded that with meticulous nerve visualization and protection during surgery, the risk of postoperative sciatic nerve injury is exceedingly low, and routine use of SSEP or electromyographic monitoring may not be necessary for experienced surgeons.
Further reading: Incidence of sciatic nerve injury in operatively treated acetabular fractures without somatosensory evoked potential monitoring – PubMed
A 2024 case report and literature review described two male patients (ages 22 and 56) who developed iatrogenic sciatic nerve palsy during acetabular fracture surgery. The injury resulted from posterior column fixation – specifically malpositioned screws or plates compressing or piercing the nerve often when the hip was flexed, causing excessive tension. Both patients underwent timely surgical exploration with hardware removal and nerve decompression. One recovered full motor and sensory function, while the other had persistent deficits at the L5/S1 level with mild pain. The study emphasizes the importance of intraoperative nerve monitoring (e.g., electromyography), early recognition, and prompt surgical intervention to optimize outcomes in such nerve injuries.
Further reading: Salvage of Iatrogenic Sciatic Nerve Injury Caused by Operatively Treated Acetabular Fractures: Two Cases and Literature Review – PubMed
Classification based on severity:
- Mild: Motor 3-4 or mainly sensory symptoms
- Severe: Motor <3 with markedly diminished sensation
Recovery based on classification:
- Mild peroneal, Mild or Severe tibial division involvement: Good prognosis
- Severe peroneal division involvement: Poor prognosis
Techniques Recommended by Letournel and Judet or prevent sciatic nerve injury during posterior approach to acetabular fixation:
- Hip and knee positioning:
- Keep the hip extended and knee flexed to reduce sciatic nerve tension.
- Use transcondylar traction to maintain this position during surgery.
- This reduced their nerve palsy rate from 18.4% to 3.3%.
- Retraction precautions:
- Avoid excessive posterior retraction when the hip is flexed.
- Do not lever retractors in the lesser sciatic notch to prevent nerve compression.
- Use Hohmann-type retractors with curved edges designed for nerve protection.
- Place the obturator internus tendon and muscle between the nerve and retractor.
- Hardware placement:
- Be cautious when drilling or placing screws near the greater sciatic notch.
- Always confirm safe instrument placement with appropriate fluoroscopic views.
Intraoperative Monitoring (SSEPs)
- Supportive evidence:
- SSEPs have been shown to reduce iatrogenic nerve injury during pelvic/acetabular surgery.
- Controversy:
- Some (e.g., Middlebrooks et al.) suggest SSEP may be unnecessary if Letournel and Judet’s precautions are followed.
- Use in high-risk patients:
- Helpful for patients with:
- Posterior wall/column fractures
- Preoperative nerve injury
- In these patients:
- SSEP changes were seen in 60% of cases.
- Posttraumatic nerve injury rate: 30% (25/83)
- Intraoperative SSEP changes: 29% (24/83)
- Helpful for patients with:
- Efficacy:
- Use of SSEPs led to a low iatrogenic neuropraxia rate: 2%
- Separate monitoring of the tibial and peroneal divisions is crucial:
- Monitoring tibial only resulted in 5% peroneal nerve injury rate
Further reading: Incidence, risk factors, and prognosis of sciatic nerve injury in acetabular fractures: a retrospective cross-sectional study – PMC