What is Kaplan’s lesion?
Metacarpophalangeal (MCP) joint dislocation: Complex (Irreducible) Dorsal
Mechanism of injury: Hyperextension injury
Involvement: Usually occurs on border digits (Index > Little finger)
Characteristic position of index finger:
- Hyperextended at MCP rests on dorsum of metacarpal
- Deviated towards middle finger
- Slightly flexed middle & distal phalanx with relaxed extensor tendons
Other features:
- Round regularly shaped mass of 2nd metacarpal head on volar surface
- Puckered skin on both sides of protruding mass – pathognomic
- Concomitant fractures of metacarpal head or proximal phalanx in upto 50%
What is the difference between simple and complex MCP joint dislocation?
Simple:
- Reducible
- Hyperextension of proximal phalanx on metacarpal head
- Flexion of Proximal Interphalangeal joint
- Xray – Proximal phalanx ~ perpendicular to Metacarpal shaft
Complex:
- Irreducible
- Bayonet positioning of proximal phalanx
- Skin dimpling in proximal palmar crease
- Xray – Proximal phalanx ~ parallel to Metacarpal shaft
What are the X-ray features of Kaplan’s lesion?
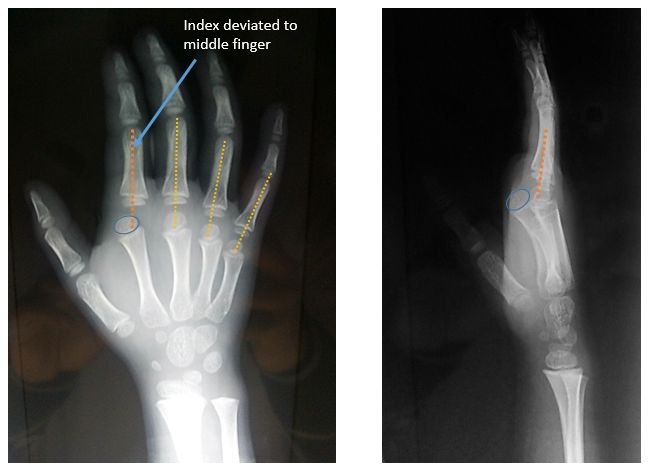
A line straight down the shaft of the proximal phalanx should intersect the metacarpal head.
Failure of the line to intersect indicates subluxation or dislocation.
Lateral view –
- Proximal phalanx lying parallel to metacarpal shaft – complex dislocation
- Proximal phalanx oriented perpendicular to metacarpal shaft – simple dislocation
Other indicators of complex dislocation:
- Widened joint space
- Ossified sesamoid in joint space (>10 yrs of age)
After whom is Kaplan’s lesion named?

The lesion was initially described by Farabeuf in 1876. Barnard had introduced this concept in English literature in 1901.
Dr. Emanuel B. Kaplan described the mechanism of injury, pathoanatomy, clinical features and method of treatemnt of this condition in 1957. In the literature, he is often titled as a legendary anatomist & hand surgeon. He has authored over 100 publications including “Functional and Surgical Anatomy of Hand (1st and 2nd Ed.)” and “Surgical approaches to Neck, Cervical spine & Upper extremity”.1
Other eponyms in his honor:
- Kaplan’s ‘cardinal line’
- Hospital for Joint Diseases named its hand fellowship after him
- NYSSH (New York Society for Surgery of the Hand) administers a prestigious annual Kaplan award
- Kaplan Institut founded in Barcelona in 1994
How common is Kaplan’s lesion?
Earlier, it was thought to be a rare occurence but recently it is often called as an uncommon or more precisely an under-reported injury in Orthopedic practice.
Emanuel B. Kaplan, in his practice of 20 years – encountered only 2 cases.
Le Clerc, in his review of literature from 1883 to 1991, collected only 10 cases.2
Pandiyan, reported 20 cases between 2010 to 2017.3
What makes the joint irreducible in Kaplan’s lesion?
Kaplan proposed a “noose theory“:
- Volar plate entrapped drosally between base of proximal phalanx and metacarpal head
- Distal and dorsal: Natatory ligament
- Proximal and palmar: Superficial transverse metacarpal ligament
- Ulnar aspect: Flexor tendons & pretendinous band
- Radial aspect: Lumbricals
Afifi et.al. examined 6 specimens where irreducible MCP dislocation was created in cadaveric hand model using an impact load.4 They concluded that:
- Volar plate is primary structure preventing reduction of dislocation – division of volar plate was necessary in all cases
- Flexor tendons, Lumbricals, STML and natatory ligaments do not contribute to irreducibility (noose theory is inaccurate)
- Radial neurovascular bundle is either radial or superficial to metacarpal head (just under the skin, making it prone to iatrogenic injury)
Why traction (in axis of metacarapal) is not used in closed reduction of MCP joint dislocation?
Traction on the affected joint can draw the entire volar plate dorsally converting simple dislocation to complex dislocation. Failure of closed reduction warrants surgery.
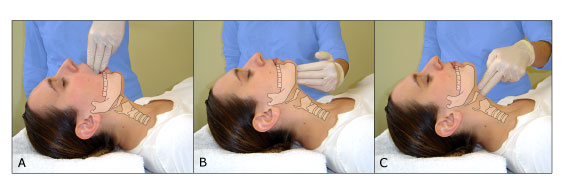
Steps of closed reduction when attempted:
- Pain management
- Flex the wrist to allow relaxation of flexor tendon
- Hyperextend the affected digit
- Apply pressure to the base of the proximal phalanx until reduction is achieved
- Apply splint
Further reading: https://www.aafp.org/afp/2013/0201/p160.html
What are the surgical approaches for management of Kaplan’s lesion?
A. Dorsal approach (Farabeuf):
- Direct exposure of the volar plate.
- No need for further release of adjacent structures to facilitate reduction.
- No danger to the neurovascular bundle.
- Concomitant fixation of the articular chip fracture is possible.
Becton et al. reported a series of 9 cases – patients treated with volar approach had a sensory loss on radial aspect of injured finger while those treated with dorsal approach had full recovery with normal function.5
B. Dorsal percutaneous approach:
- Anesthesia: LA
- Metacarpal dorsal surface is palpated with deep palpation
- Using 11 size blade, soft tissue that is present over the dorsal surface of Metacarpal shaft is incised longitudinally till the Metacarpal neck
- This incision will usually incise dorsally displaced volar plate which lies as a block
- With gentle traction and corrective manipulation, dislocation is reduced by easy means 6
Criticism of Dorsal approach:
Longitudinal splitting of volar plate causes:
- Delay in recovery
- Needs more immobilization
- Leads to instability of the joint
But this seems to be only theoretical – studies show no difference in functional outcome.
C. Kaplan’s Volar approach – Triple incision:
- 1st incision – exposes the area of dislocation
- 2nd incision – made above the metacarpal head, divides volar plate and natatory ligament
- 3rd incision – made below the metacarpal head, divides Short Transverse Metacarpal Ligament (STML)
Advantage: Volar plate can be repaired.
D. Lateral approach:
Advantages:
- Visualization of both volar and dorsal structures – Fixation of volar plate + Osteochondral fractures
- Operative scar – reduced risk of tendon adhesions and scar retractions that may limit joint movement
Risks: Nerve and vessel injury 7
E. Combined volar and dorsal approach:
May be necessary for late presentation (>3 weeks) 8
How is rehabilitation instituted for Kaplan’s lesion?
- Immobilization of the joint in 30 degrees of flexion X 2 weeks
- Active ROM in removable dorsal extension block splint (to prevent last 10 degrees of extension)
- At 4 weeks the splint is used only for protection
- At 6 weeks splint is discontinued 9
What are the complications of Kaplan’s lesion?
- Stiffness
- Arthritis
- Osteonecrosis of metacarpal head
- Premature closure of physis
- Digital nerve damage

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.