Hypertension in pregnancy is one of the major cause of maternal, fetal and neonatal mortality and morbidity in both the developing and developed nations. About 10-15% of pregnancies are accompanied by hypertension and if these are detected early and effective interventions are performed, the prognosis is good.
A. HISTORY FOR HYPERTENSION IN PREGNANCY:
Ask relevant questions necessary to identify the risk factors:
| Maternal general | Age over 40 years |
| Obstetric history | Previous pre-eclampsia |
| Previous gestational hypertension | |
| Multiple pregnancies | |
| Nulliparity or interpregnancy interval greater than 10 years | |
| Artificial insemination with donor sperm | |
| Pre-existing conditions | Chronic hypertension |
| Diabetes mellitus | |
| Congenital heart conditions: coarctation of the aorta, transposition of great vessels, pulmonary atresia with VSD and pulmonary stenosis | |
| Chronic renal disease | |
| Thrombophilia, such as antiphospholipid syndrome | |
| Increased body mass index | |
| Migraine |
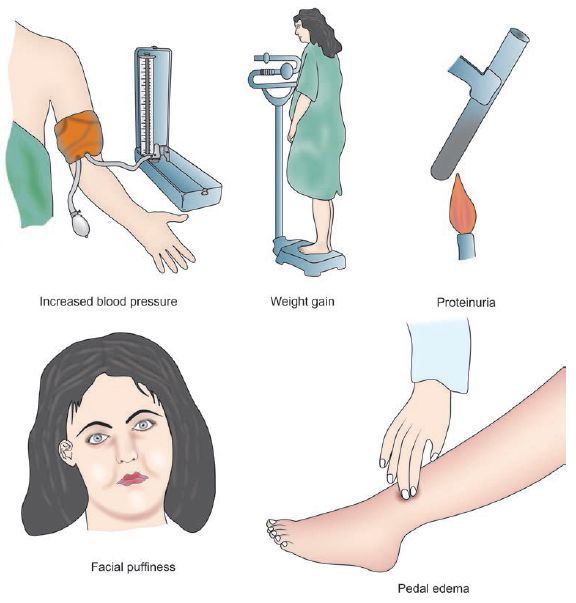
Identify mild and alarming symptoms of hypertension in pregnancy:
1. Mild symptoms (Edema):
This can be due to proteinuria (glomeruloendotheliosis). Since, edema is a universal finding in pregnancy, pathology may be indicated by:
- Persistent ankle edema in the morning
- Tightening of rings on fingers of hand
- Facial puffiness
- Vulval edmea
2. Alarming symptoms:
These alarming symptoms indicate severe pre-eclampsia or it’s complications like eclampsia and end-organ dysfunction:
| Symptoms | Description | Significance |
| Headache | Frontal or Occipital; unrelieved by simple analgesics | Cerebral edema, CNS hemorrhage |
| Visual disturbance | Blurring, diplopia, scotoma | Retinal infarction , Occipital lobe damage (vasogenic edema), Retinal detachment |
| Acute abdominal pain | Epigastric or right upper quadrant; may be associated with vomiting or hematemesis | Hemorrhagic gastritis, Subcapsular hemorrhage in liver, Hepatic necrosis, HELLP syndrome |
| Diminished urine output | Oliguria i.e.<400 ml in 24 hours | Reduced plasma volume (Renal hypoperfusion), Ischemic acute tubular necrosis |
| Dyspnea | Shortness of breath | Acute pulmonary edema, ARDS (Acute Respiratory Distress Syndrome), Penumonia (Aspiration or Infective) |
| Reduced fetal movements | Intrauterine growth restriction (IUGR) or Oligohydramnios | |
| Convulsions or fits What is Status eclampticus?When convulsions occur in quick succession without remission |
1. Premonitory stage (30 seconds): Loss of consciousness, eyeballs roll/turn to one side/fix 2. Tonic stage (30 seconds): Opisthotonus, flexed limb, clenched hands, respiration ceases, tongue protrudes between teeth, cyanosis, fixed eyeballs 3. Clonic stage (1-4 minutes): Generalized twitching starting from face, Tongue bites and blood stained frothy secretions in mouth, Stertorous breathing 4. Stage of coma |
Eclampsia – due to cerebral irritation and excessive release of glutamate (excitatory neurotransmitter) resulting from:1. Cerebral anoxia (vasospasm)2. Cerebral edema
3. Cerebral dysrhythmia |
B. EXAMINATION FOR HYPERTENSION IN PREGNANCY:
1. General Physical Examination:
a. Raised Blood Pressure (Hypertension):
- Position: Avoid measuring blood pressure in supine position lying on back (Supine hypotension syndrome can give false reading)
- Precautions:
- Choose the right size of cuff (encompassing 40% of arm circumference)
- The woman should not use tobacco or caffeine within 30 minutes of the measurement.
- Significant reading: >140/90 mmHg
b. Proteinuria in Dipstick test:
- Qualitative test and not very accurate
- Reagent strip is dipped into fresh urine specimen (first morning specimen is not preferred due to possibility of false high reading) and immediately removed from the specimen
- Assess the color change in reagent strip after 1 minute and compare with the index provided by manufacturer (often on the sides of bottle)
- Grading based on visual assessment: Trace; 1+ = 0.3 g/L; 2+ = 1 g/L; 3+ = 3 g/L; and 4+ = 10g/L
- Significant reading: >1+
c. Edema: Pitting edema localized to especially to the ankle or may be generalized
d. Weight gain: More than 5 lb/month or more than 1 lb/week is significant
e. Signs of pulmonary edema: Crackles, S3 gallop, etc.
f. Petechiae: May indicate HELLP syndrome, Thrombocytopenia, DIC (Disseminated Intravascular Coagulation)
g. Ankle clonus or Hyper-reflexia: Indicates excessive neuromusuclar irritability with possiblity of progression to eclampsia
h. Knee jerks: Reduction or absence is a sign of magnesium toxicity which is used for seizure prophylaxis in severe pre-eclampsia and eclampsia
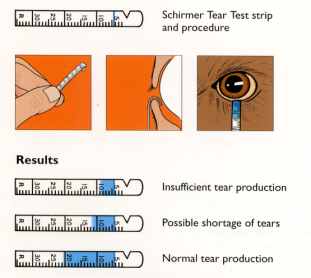
i. Papilledema (Fundoscopy): Increased ICP associated with malignant hypertension
2. Abdominal examination:
Evidences of chornic placental insufficiency includes:
- Fundal height less than the estimated on the basis of Last Menstrual Period (Intrauterine Growth Restriction or IUGR)
- Uterus may appear full of fetus (Oligohydramnios)
C. DIFFERENTIAL DIAGNOSES FOR HYPERTENSION IN PREGNANCY
On the basis of onset of hypertension, measurement of blood pressure, presence of proteinuria or seizures – establish your provisional diagnosis, which may be:
- Chronic hypertension
- Gestational hypertension
- Pre-eclampsia
- Severe pre-eclampsia
- Eclampsia
- Pre-eclampsia superimposed on Chronic hypertension
Diagnostic criteria and Pathophysiology of Pregnancy induced Hypertension
If a diagnosis of Eclampsia is made, conditions associated with convulsions must be kept in mind, and relevant symptoms and signs must be looked for during history and examination:
- Epilepsy
- Hysteria
- Encephalitis (Perform lumbar puncture if supsected)
- Meningitis (Perform lumbar puncture if suspected)
- Puerperal cerebral thrombosis
- Poisoning (Send urine toxicology if suspected)
- Cerebral malaria
- Intra-cranial tumors (Head CT may be useful)
D. INVESTIGATIONS FOR HYPERTENSION IN PREGNANCY:
| Urinalysis | Proteinuria – dipstick protein of>1+necessitates follow up with a spot urinary protein:creatinine ratio |
| Abnormal is >30 mg/mmol | |
| Full blood count | Haemolytic anaemia |
| Thrombocytopaenia | |
| <100×109/L may indicate DIC | |
| <50×109/L may indicate need for platelet transfusion | |
| Haemolytic anaemia with thrombocytopaenia may indicate HELLP syndrome | |
| Increased Hematocrit (HCt) may indicate decreased plasma volume | |
| Electrolytes and creatinine | Elevated creatinine (>1 mg/dl) |
| Liver function tests | Transaminases>70 IU/L consistent with hepatic parenchymal damage |
| Raised bilirubin from haemolysis | |
| Lactate dehydrogenase | Raised in haemolysis |
| Abnormal coagulation profile | Evidence of DIC (↓ fibrinogen,↑ FDPs) DIC likely in placental abruption, and hepatic subcapsular haematoma |
| Serum urate | > 4.5 mg/dl is a biochemical marker of pre-eclampsia |
| Blood grouping and hold | For RBC and platelet transfusion |
| Fetal assessment | Daily fetal kick count, Ultrasound for oligohydramnios or fetal growth restriction |
| CTG for fetal distress, Umbilical artery flow veolcimetry, Biophysical profile |
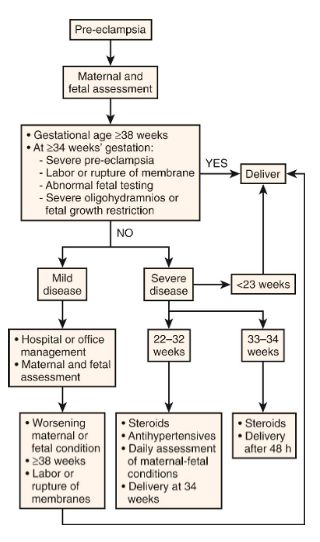
E. TREATMENT OF PRE-ECLAMPSIA:
1. Bed rest (Preferably in Left lateral position):
- Increases renal perfusion (diuresis)
- Increases uterine perfusion (improves placental perfusion)
- Reduces blood pressure
2. Diet: Well balanced diet rich in protein (100 gm/day) and calories (1600 kcal/day)
3. Diuretics: Diuretics should be used judiciously as maternal circulatory volume is already reduced. Frusemide (Lasix) oral is indicated for –
- Cardiac failure
- Pulmonary edema
- Diazoxide therapy (associated with fluid retention)
- Massive symptomatic edema
4. Antihypertensive therapy:
a. Short-term control of Blood Pressure (BP): If BP ≥ 160/110 mmHg or MAP ≥ 125 mmHg
| Drug | Dose | Onset | Adverse effects / Comments |
| Labetalol | 10–20 mg IV every 10 min (max. 300 mg) Maintenance: 40 mg/hr |
5 min | It is a combined α and β blocker Bronchospasm in asthmatics, Tremor Heart block |
| Hydralazine | 5 mg IV every 30 min (max. 30 mg) Maintenance: 10 mg/hr |
10 min | It is an arterio-dilator. Hypotension, Palpitations, Lupus like syndrome Neonatal thrombocytopenia |
| Diazoxide | 15–45 mg IV; may be repeated in 5 min (max. 300 mg) |
5 min | It is a Potassium channel opener. Flushing, Hyperglycaemia Tachy- or bradycardia Sodium and water retention |
| Nifedipine | 10–20 mg PO; may be repeated in 30 min (max. 240 mg/24 hr) | 10 min | It is a calcium channel blocker (arterio-dilator) Tachycardia, Flushing, Hypotension, Inhibition of labor Not used in aortic stenosis |
| Nitroglycerine | 5 µg/min IV | 0.5-5 min | Only used when other drugs have failed. It is a venodilator. Tachycardia, headache, Methemoglobinemia Not to be used in hypertensive encephalopathy (↑ICP) |
| Soidum Nitroprusside | 0.25-5 µg/kg/min IV | 0.5-5 min | Only used when other drugs have failed. It is a direct arterial and venous dilator. Severe hypotension, Fetal toxicity (cyanide, thiocyanate) |
b. Oral antihypertensives: For BP falling out of severe level and persistent rise in BP during continued pregnancy or induction of labor
- Oral Methyldopa (Central and peripheral anti-adrenergic): Side effects like Postural hypotension, Postpartum depression
- Oral Nifedipine (Calcium channel blocker): Side effects like edema, dizziness
- Others: Oral Labetolol, Oral Hydralazine
Note: ACE inhibitors and Angiotensin Receptor Blockers (ARBs) are not indicated in pregnancy due to teratogenecity in 1st trimester, fetal renal failure and oligohydramnios.
5. Progress monitoring:
- Daily detailed examination
- Regular weight measurement at weekly intervals
- Daily dipstick test for proteinuria (24 hour estimation if significant)
- Blood pressure measurement to be done every 4 hourly (at least four times a day)
- The following investigation to be done on weekly basis: Hematocrit with platelet count, RFT (blood urea; serum uric acid; and serum creatinine); LFT (AST, ALT and LDH) and ophthalmoscopic examination.
F. TREATMENT OF ECLAMPSIA:
- Maintain Airway, Breathing and Circulation
- Left lateral decubitus position (reduces pressure on Inferior venacava, enhancing cardiac and renal output)
- Suction oropharynx, Protect from injury, Avoid restraining the patient
- Arrest convulsions with Magnesium sulfate regimen (Use phenytoin if contraindication to MgSO4 are present)
- Add IV antihypertensives (Hydralzine or labetalol or calcium channel blockers or nitroglycerine) if BP remains > 160/110 mmHg (Hypertensive crisis)
- Fluid managment:
- Ringer Lactate not exceeding 2 L in 24 hours
- IV frusemide 40 mg only in cases of acute pulmonary edema
- For status eclampticus: Thiopentone sodium 0.5 gm dissolved in 20 ml of 5% dextrose given IV very slowly
- Intubate for airway protection/hypoxia or if seizures refractory to intervention
- Organize investigations
- Delivery of baby (only definitive treatment): No expectant management is recommended regardless of gestational age and must be performed within 6-8 hours if fits are not controlled
- Induction of vaginal delivery is recommended
- Artificial Rupture of Membrane (ARM)
- Oxytocin
- If fits is controlled and cervix is unripe: PGE2 (Dinoprostone) gel can be used
- Cesarean section is indicated if:
- Uncontrolled fits despite of therapy
- Unconscious patient and poor prospect of vaginal delivery
- Obstetric indications
- Women often go into spontaneous labor after onset of seizures, and/or have a shorter duration of labor
- Induction of vaginal delivery is recommended
- Intrapartum monitoring:
- Vitals are recorded half hourly
- Urine output, respiratory rate and Deep tendon reflex for Magnesium toxicity
- Fetal heart rate
G. EARLY POSTPARTUM MANAGEMENT FOR HYPERTENSION IN PREGNANCY:
- Postpartum hemorrhage (PPH) prophylaxis
- Continue MgSO4 as discussed in the regimen
- Neonatal care till mother is stable
- Titration of antihypertensive agents
- Prophylactic antibiotics
Submitted by: Sulabh Shrestha
This article is only for academic purpose and should not be used as a medical advice.
thanx. very insightful
Thanks for sharing the valuable information. I must agree that hypertension or high blood pressure during pregnancy can lead to serious conditions. It can even lead to premature delivery, placental abruption or other cardiovascular disease. It is one of the most common conditions that encountered in women during pregnancy. So a pregnant women need to take extra care during pregnancy. Few days back, I got to read this similar blog Which is as interesting as yours on the same topic, you can read it here: http://cloudninecare.com/blog/hypertension-and-pregnancy-know-the-facts/