What is Fibromyalgia?
Fibromyalgia is a chronic illness characterized by many symptoms that occur all at once:
1. Widespread pain
2. Fatigue
3. Sleep problems
4. Cognitive disturbances (concentration, memory)
5. Altered mood (anxiety, depression)
6. Other symptoms: headache, digestive disorders, dizziness, muscle spasms, chills, low-grade fever, ringing in the ears, dry mouth and eyes, widespread itching.
Fibromyalgia has a fluctuating course, with periods of improvement and flare-ups, which depend on many different circumstances and are distinct in each patient.
How common is Fibromyalgia?
Fibromyalgia affects upto 5% of the world population. The incidence is greater in Europe (2.64%) than in America (2.41%) or parts of Asia (1.62%).
The incidence is higher in women than in men, and the age range in which FM generally appears is between 30 and 35 years.
How Fibromyalgia develops?
Malfunctions in the neurotransmitters (serotonin, noradrenaline, adrenaline, dopamine, etc.) lead to a situation in which some stimuli are perceived more strongly than usual, thus producing the characteristic, widespread aches and pains of fibromyalgia. This malfunction also leads to other symptoms of fibromyalgia.
Any stressful life event can act as a trigger in a genetically predisposed individual – an accident, an operation, being assaulted, menopause, problems at home or work, etc.
How is Fibromyalgia diagnosed?
The presence of fibromyalgia does not rule out other diseases. The presence of other diseases does not rule out fibromyalgia. No lab tests or other diagnostic tests are required for its diagnosis.
The ACR’s updated fibromyalgia diagnostic criteria from 2010 – suggests using questionnaires that assess pain and related symptoms, called the widespread pain index (WPI) and symptom severity scale (SSS).
The WPI asks where you felt pain in specific areas of the body, noting a “1” for each area. The SSS assesses how the pain feels in terms of fatigue, cognitive symptoms, and how you feel when you wake up, on a scale of 0 (no problems) to 3 (severe and continuous).
Doctors diagnose fibromyalgia based on the following general guidelines:
1. Using the Widespread Pain Index and Symptom Severity Scale when (WPI) ≥7 and the Symptom Severity Scale (SSS) score ≥5, OR WPI 4–6 and SSS score ≥9.
2. Generalized pain, defined as pain in at least four of five regions (left upper, right upper, left lower, right lower, low back) is present.
3. Symptoms have been present and consistent for at least 3 months.
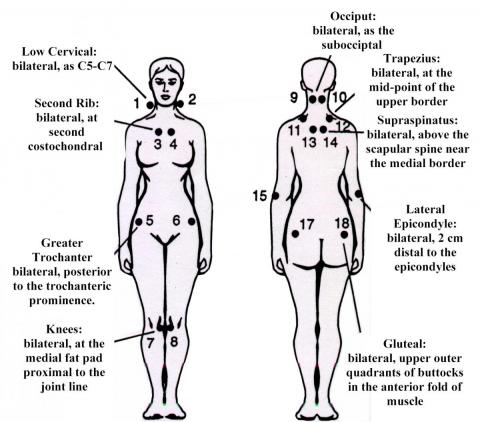
4. Counting tender points (not required in new criteria)
How is Fibromyalgia treated?
There is no curative treatment for fibromyalgia. Evidence supported treatments for fibromyalgia are:
1. Information and education
2. Regular exercises
3. Some types of psychotherapy
4. Some medicines:
Antidepressants and anticonvulsants act on nervous system and have shown beneficial effects.
There are many types of antidepressants and anticonvulsants, with different effects in each patient; trial and error are the only way to find out which is best for you. Painkillers or analgesics, such as paracetamol, will reduce your pain. This is the medicine you should take as soon as you start feeling pain. Since fibromyalgia follows a fluctuating course, it is a good idea to come off as many medicines as possible when you’re feeling a bit better. The reasoning behind this is that, when you have another flare-up that requires medication, you’ll have a better response to treatment.
Recommended readings and References:
- A Beginner’s guide to Fibromyalgia
- Queiroz LP. Worldwide epidemiology of fibromyalgia. Curr Pain Headache Rep. 2013 Aug;17(8):356. doi: 10.1007/s11916-013-0356-5. PMID: 23801009.