How to answer definitions ?
Definitions are often asked in the exams – both in theory exams and viva-voce. As the content is vast, mugging them up is not a good idea. If you have a good understanding over the topic, you can write down a good definition by including following things wherever possible:
- Basic pathophysiology or process: Nature of infection, Premalignant condition, Benign/malignant neoplasm, Localized collection, etc.
- Involved structures: Layers of skin, Structures invaded by malignancy, etc.
- Peculiar identifying feature: certain size, duration, etc.
- Can include: Diagnostic clinical feature(s), Indication, The difference from a common differential diagnosis
Example:
Delayed Primary Closure (DPC): Surgical closure of a wound (1) 3-5 days after the thorough cleansing or debridement of the wound bed (3) when there is contamination or high risk of contamination (4).
Aneurysm: Pathological, localized, permanent dilation of an artery (1) to >1.5 times (3) the original diameter involving all 3 layers (2 and 4 – mentions the involved layers and also differentiates from pseudoaneurysm which doesn’t involve all the 3 layers of arterial wall) of its parent wall.
Locally Advanced Breast Carcinoma (LABC): Malignant neoplasm of the breast (1) that has not spread to distant sites i.e. Mo (3) but may be one of the following (2):
- Primary tumor >5 cm (T3)
- Chest wall and/or skin involvement including inflammatory carcinoma (T4)
- Ipsilateral fixed axillary lymph nodes and/or internal mammary nodes or infraclavicular or supraclavicular nodes (N2 or N3)
How to answer causes and etiologies ?
List down the causes in a systematic manner after classifying them. The general rules for doing them are –
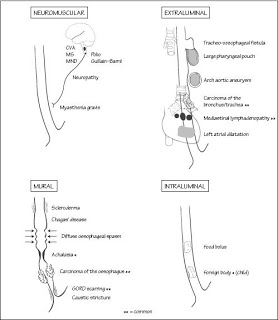
a. Causes involving conditions in a hollow viscus:
- Mechanical:
- In the lumen: usually stones, foreign body or worms
- In the wall: usually inflammatory or neoplastic conditions and strictures
- Outside the wall: usually enlargement of adjacent structures, lymph nodes or abnormal protrusions
- Non-mechanical: usually neuromuscular and metabolic causes
Example:
Causes of dysphagia:
- Mechanical:
- In the lumen: Foreign body (dentures, coin)
- In the wall:
- Inflammation: Infectious esophagitis, tuberculosis
- Neoplasm: Carcinoma esophagus
- Inflammatory or post-irradiation strictures
- Outside the wall: Aortic aneurysm, retropharyngeal abscess, thyroid enlargement, cardiomegaly, mediastinal nodes
- Non-mechanical: Myasthenia gravis, Polymyositis, Achalasia, Scleroderma, Cranial nerve IX and/or X lesions
Causes of intestinal obstruction:
- Mechanical:
- In the lumen: gallstones, impacted feces, meconium, worms, foreign body
- In the wall: Inflammatory or malignant strictures, Diverticulitis
- Outside the wall: Adhesions and bands, cancers, hernia, volvulus
- Non-mechanical:
- Paralytic ileus: postoperative abdominal surgery, mesenteric ischemia, hypokalemia, hypothyroidism, etc.
- Pseudo-obstruction
b. For answering all other etiologies:
Use a surgical seive and remember them using a mnemonic like “MEDIC HAT PIN”
- Metabolic
- Endocrine
- Degenerative
- Infective
- Congenital
- Hematological
- Autoimmune
- Trauma
- Psychological
- Inflammatory
- Neoplastic
Example:
Causes of splenomegaly –
- Idiopathic: Idiopathic thrombocytopenic purpura
- Vascular: portal vein obstruction, Budd-Chiari syndrome, haemoglobinopathies (Sickle-cell disease, thalassemia)
- Infective: AIDS, mononucleosis, septicaemia, tuberculosis, brucellosis, malaria, infective endocarditis
- Traumatic: haematoma, rupture
- Autoimmune: rheumatoid arthritis, SLE
- Metabolic: Gaucher’s disease, mucopolysaccharidoses, amyloidosis, Tangier disease
- Inflammatory: sarcoidosis
- Neoplastic: CML, metastases, myeloproliferative disorders
Note: Always highlight the commonest and more common causes when using these systems for answering.
How to answer the clinical features of the given disease conditions ?
Classify into symptoms (subjective complaints and remember to elaborate using a mnemonic – SOCRATES; elaborate the main complaint and keep others as associated features) and signs (objective findings) expected in the disease condition; Use eponymous signs and elaborate in one line whenever possible –
Example:
In Acute Appendicitis –
A) Symptoms:
- Site of pain: Right iliac fossa
- Onset of pain: Acute over 24-48 hours
- Character of pain: Initially dull visceral pain, later becoming sharp and localized due to parietal peritoneum involvement
- Radiation or migration: Migrating to RIF from umbilicus
- Associated symptoms: Anorexia, Nausea/vomiting, Fever, etc. (Murphy’s triad – pain, vomiting and fever)
- Timing: No association
- Exacerbating and relieving factor: As in all cases of peritonism – increased by movement and coughing and relieved partially by rest
B) Signs:
- Pointing sign, Blumberg’s sign, Obturator sign, Psoas sign, Rovsig’s sign, Sherren’s triangle hyperesthesia, Rectal wall tenderness on PR, etc.
How to answer the investigations for given disease conditions ?
Always mention the expected findings of the tests and answer in the following order –
- Investigations to prove diagnosis
- Investigations to rule out differential diagnoses
- Routine investigations, pre-operative investigations and Investigations to rule out or identify complications
- Investigations for monitoring the disease
Example:
In Acute Pancreatitis –
1. Investigations to prove diagnosis:
- Serum amylase and lipase: Increased by atleast 3 times
- Abdominal USG: Can detect gallstone, biliary obstruction and pseudocyst formation
- CECT abdomen: Confirms the diagnosis and aids in providing prognosis to the disease
- Plain AXR: Sentinel loop sign, Colon cut-off sign, Renal halo sign, Pancreatic calcifications
- LFT: can suggest if the cause is gallstone or alcohol
2. Investigations to rule out differential diagnosis:
- ECG: To rule out MI
- Plain abdominal X-ray erect and supine: To rule out perforation
- Stool for occult blood: To rule out mesenteric ischemia
- USG abdomen: To rule out cholecystitis
3. Routine, Pre-op investigations and Investigations to identify complications:
- CBC and HCt: resembling SIRS or septic shock
- RFT: to rule out renal failure due to hypovolemia
- RBS: Hyperglycemia
- Serum albumin: Decreased
- Serum calcium: Decreased
- ABG: Metabolic acidosis
- Plain Chest X-ray: Pleural effusion, ARDS
- Pre-op investigations: Serology, Blood grouping and cross-matching
4. Investigations for monitoring disease progression: CBC and HCt, ABG, Serum calcium, RFT, etc.
How to answer treatment for a give disease conditions ?
Whenever possible, follow the following order –
- Firstly: Stabilization of vitals (Go with ABC approach as in BLS) and emergency management
- Secondly: Conservative management (if possible)
- Thirdly: Medical and Surgical management
Example:
For treatment of nephrolithiasis –
Firstly: Manage acute pain, UTI and deranged renal function if present
- Analgesics: NSAIDs (1st choice), Opioids (2nd choice)
- Anti-emetics: If vomiting
- Alpha-blockers: reduces recurrent colic
- IV hydration
- Antibiotics for UTI
- Percutaneous nephrostomy for decompression may be required
Secondly: Conservative management if possible
- Adequate water intake (atleast 2 litres per day)
- Exercise
- Urine alkalizer +/- allopurinol for suspected urate stones
- Periodic evaluation
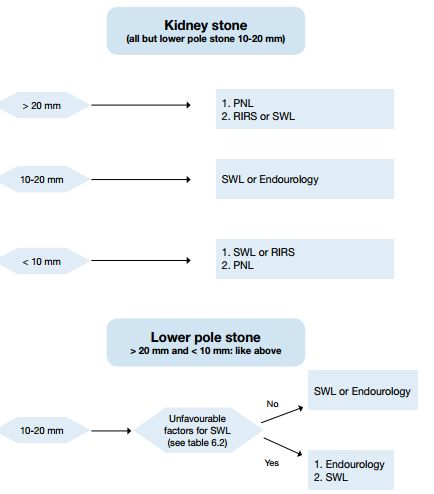
Thirdly: Medical or Surgical management with indications
Replicate contents from textbooks into concise flowcharts whenever possible.
This has 2 advantages:
- Saves time
- Easy to the examiner’s eyes.
How to answer the asked procedures ?
Be concise and answer in following order – Indications, Requirements, Description of procedre site, Procedure (Position, Anesthesia, Incision, Dissection, Performing targeted procedure, Closure), Confirm correct placement and if the intervention is functional and Complications
Example:
Explaining Chest tube insertion –
- Indications:
- Traumatic hemothorax
- Traumatic pneumothorax
- Drainage of empyema
- Following thoracotomy
- Requirements: Sialistic chest tube drain, Underwater seal drainage bag, Inj. 1% lignocaine, Straight and curved clamp, Suture and dressing set
- Working site: Safety triangle – bounded by anterior border of latissimus dorsi, posterior border of pectoralis major, superior border of 5th rib
- Procedure:
- Anesthesia: Backrest lifted to 45 degrees
- Anesthesia: LA 1% inj. lignocaine (skin to parietal pleura)
- Incision: Over safety triangle
- Dissection: Intercostal muscles separated using curved clamp, Blunt dissection with finger down upto pleura
- Chest tube inserted towards apex for pneumothorax and towards base for effusion
- Chest tube clamped and closed end cut-off to connect to a water seal draiange bag (2-3 cm inside water)
- Drain fixed – stictch in a circular fashion
- Sterile dressing pad applied
- Confirmation:
- Correct placement: Chest X-ray
- Functional: Tidalling, Bubbles in the underwater seal drain (pneumothorax)
- Complications:
- Hemorrhage
- Intercostal neurovascular injury
- Lung and mediastinal injury
- Infection
How to answer the complications of a procedure or surgery ?
Classify and present as following:
1. Per-operative:
- Surgery-related: Anatomical injury (Vessels and Organs)
- Anesthesia related
2. Post-operative:
- Immediate (<24 hrs):
- Local: Reactionary hemorrhage
- General: Asphyxia (Airway obstruction with tongue fall or aspiration of vomitus)
- Early (upto 3 weeks):
- Local:
- Paralytic ileus (abdominal surgeries)
- Infection (wound, peritonitis, pelvic, subphrenic)
- Secondary hemorrhage
- Dehiscence (wound, anastomosis)
- Obstruction (fibrinous adhesions)
- General:
- Pulmonary: Collapse, Bronchopneumonia, Emboli
- Urinary: Retention, ATN
- DVT
- Enterocolitis
- Bedsores
- Parotitis
- Local:
- Late (>3 weeks):
- Local:
- Obstruction (fibrous adhesions)
- Incisional hernia
- Persistent wound sinus
- Recurrence of original lesion
- Scar probles (hypertrophic scars, keloid)
- General: After extensive resections or gastrectomy
- Anemia
- Vitamin deficiency
- Steatorrhea and/or diarrhea
- Dumping syndrome
- Osteoporosis
- Local:
Example:
After thyroidectomy –
1. Per-operative:
- Surgery related:
- Vascular injury: Primary hemorrhage from superior or inferior thyroid artery, thyroid ima. artery, carotid artery, jugular vein
- Nerve injury: External laryngeal nerve
- Solid organ injury: Injury to parathyroid gland, apex of lung
- Hollow viscus injury: Trachea, esophagus, larynx
- Anesthesia related
2. Post-operative:
- Immediate:
- Local: Reactionary hemorrhage, Asphyxia due to hematoma, Hoarseness due to recurrent laryngeal nerve injury
- General: Asphyxia, Thyrotoxic crisis
- Early:
- Local: Wound infection, Laryngeal edema
- General: Chest infection
- Late:
- Local: Scar, Stitch granuloma
- General: Thyroid and parathyroid insufficiency

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.