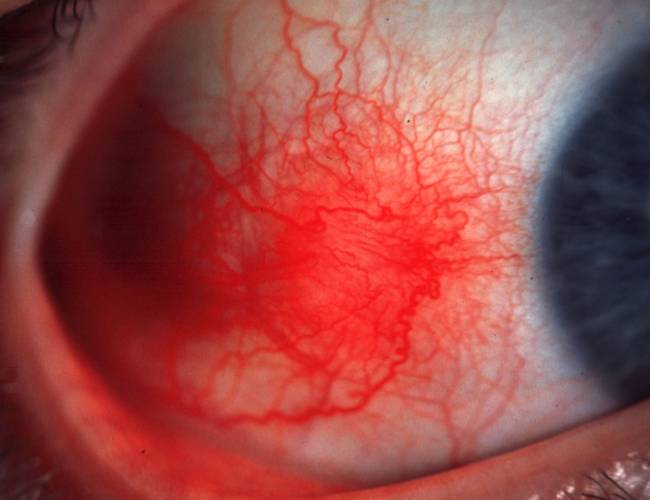
This is a case of nodular episcleritis.
Definition of Episcleritis: Episcleritis is defined as the benign recurrent inflammation of episclera and tenon’s capsule.
Types of Episcleritis:
- Diffuse episcleritis
- Nodular episcleritis
Epidemiology:
- Common in females compared to males
- Common in young adults
Etiology:
- Non-specific immune response to irritants
- Idiopathic (mostly)
- Rheumatoid arthritis (RA)
- Sjogren’s syndrome
- Systemic Lupus Erythematosus (SLE)
- Herpes Zoster
- Tuberculosis
- Syphilis
- Coccidiodomycosis
- Rosacea
Differential diagnoses:
- Phlycten
- Inflamed piguecula
- Scleritis
- Sclerosing keratitis
Episcleritis periodica fugax: Fleeting and repeated attacks of episcleritis
Distinguishing Episcleritis from Scleritis:
| Points | Nodular episcleritis | Nodular scleritis |
| Pain/Tenderness | Mild | Severe, generalized, periocular |
| Injection | Affects superficial episcleral plexus | Affects deep sclera plexus |
| 2.5% phenylephrine | Blanches | Untouched |
| Color of involved site | Bright red | Bluish or dusky |
| Nodule | Conjunctiva freely mobile over it and traversed by vessels | Diffuse and fixed |
| Scleral affection | No | Yes, repeated attacks may lead to necrosis and ectasia |
| Corneal complications | Minimal | Seen in 30-40% cases |
| Uveitis | Occasional mild iritis | Present in 30% cases |
Treatment of Episcleritis:
- Artificial tears and/or Topical vasoconstrictor antihistamine drop (naphazoline/pheniramine)
- Unresponsive cases: Mild steroid drop
- Rarely, oral NSAID may be needed
Note: Warn the patient that episcleritis can recur.
Anatomy of Episclera and Sclera:
| Episclera | Sclera | |
| Character | “Above” sclera | Collagen and proteoglycan in criss-corss arrangement |
| Loose vascular complex between conjunctiva and sclera within Tenon’s capsule | Thickness: 1-1.35 mm near optic nerve and thins anteriorly (thinnest immediately behind extraocular muscle insertion) | |
Superficial and deep plexus (from anterior and posterior ciliary arteries)
|
AvascularHave endothelial pumps
Posteriorly continuous with dural sheath |
|
| Functions | As synovial membrane for smooth movement of eye | Protective covering |
| Nutrition to avascular sclera | Blocks extraneous light to enter globe | |
| Site of insertion of Extraocular muscles | ||
| Involvement | Nearly always in Scleritis | Never in Episcleritis |
Scleritis: It is the chronic inflammation of sclera proper and is rarer than episcleritis. It is more common in females and elderly patients (40-70 years). The causes of scleritis are:
- Collagen vascular disorders: Rheumatoid arthritis, Polyarteritis nodosa, Wegner’s granulomatosis, SLE, Ankylosing spondylitis
- Metabolic: Gout, thyrotoxicosis
- Infections: Herpes zoster ophthalmicus, Chronic staphylococcal or streptococcal
- Granulomatous: Tuberculosis, Syphilis, Sarcoidosis, Leprosy
- Miscellanous: Chemical burns, VKH syndrome, Bechet’s disease, Rosacea
- Surgical
- Idiopathic
Types of scleritis:
A. Anterior scleritis:
- Non-necrotizing (commonest): Diffuse or nodular
- Necrotizing:
- with inflammation: severe pain, choroid visible through transparent sclera
- without inflammation (scleromalacia perforans): usually asymptomatic and associated with rheumatoid arthritis; uveal dehiscence and globe rupture with minor trauma
B. Posterior scleritis: Usually not associated with systemic disease
- Synonyms: Sclerotenonitis, Periscleritis, Anterior inflammatory pseudotumor
- May mimic an amelanotic choroidal mass
- Clinical features: Severe pain, proptosis, restricted extraocular movements, sometimes uveitis, exudative retinal detachment, retinal hemorrhage, choroidal folds, choroidal detachment
Investigations: ESR, Chest X-ray, RF, VDRL, ANA, serum uric acid, mantoux test, USG-B scan (to detect posterior scleritis) etc.
Complications:
- Scleral melt
- Corneal ulceration
- Secondary glaucoma
- Complicated cataract
- Exudative Retinal detachment (Posterior scleritis)
Differential diagnosis:
- Other causes of red eye
- Posterior scleritis: Masquerade syndrome with malignant melanoma of choroid, lymphoma, multiple myeloma
- Anterior necrotizing scleritis: Invasive squamous cell carcinoma of conjunctiva
Treatment:
Local and General: Topical steroids, atropine, hot fomentation
If infectious, culture and treat as appropriate
If non-infectious:
- Oral NSAID (ibuprofen or indomethacin) for 2 months
- If recalcitrant: Oral steroid (prednisolone) and taper after 2 months
- If recalcitrant: Steroid sparing immunosuppresants (40-60% success) OR 1 time subconjunctival steroid injection (90% success)
- Still recalcitrant: Anti-TNF drug