| Lesions | Age | Demographics | Site | Presentation | Imaging | Treatment | Comments |
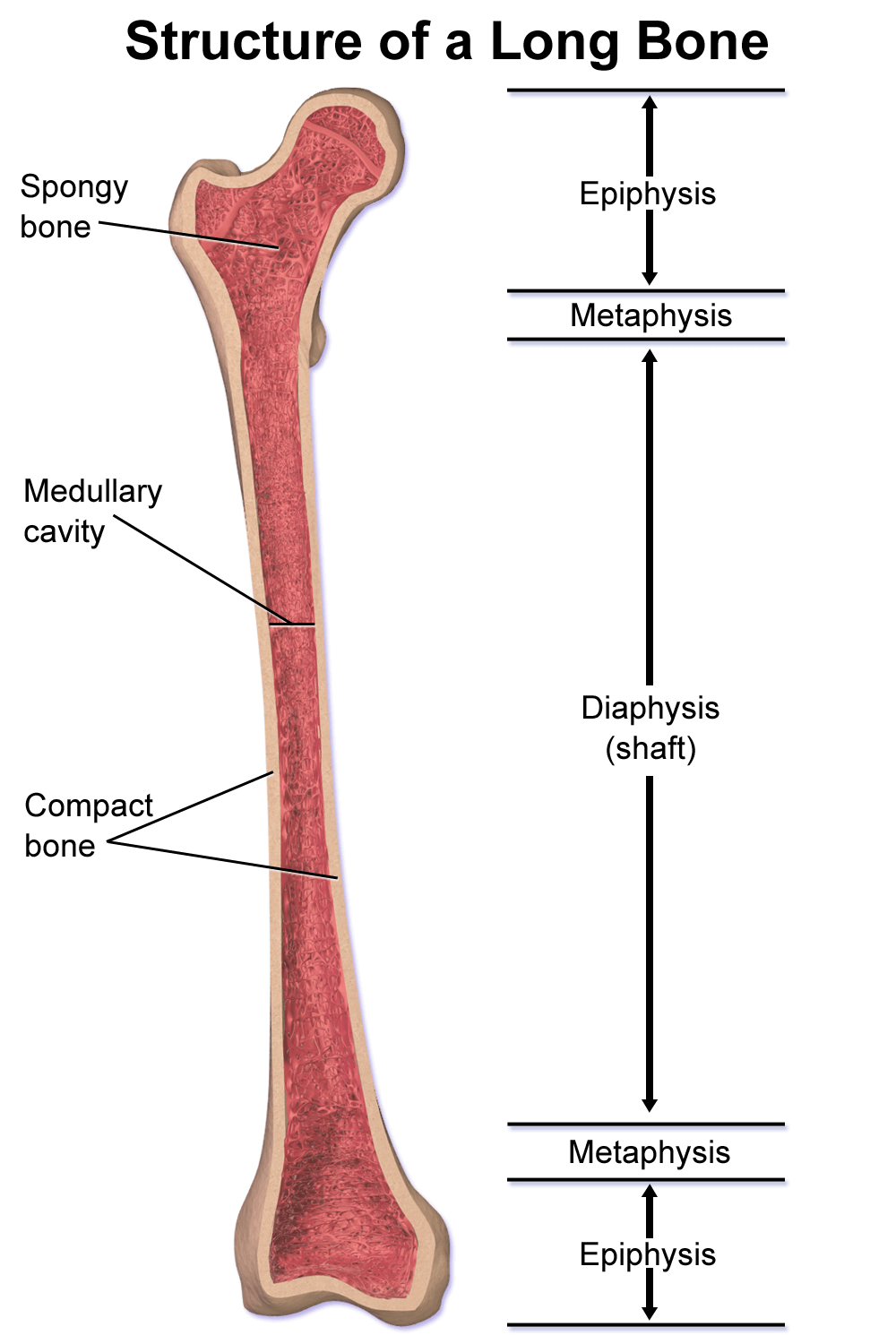
| Acute Osteomyelitis | Bimodal (<2 years and 8-12 years) | M:F = 2:1 | Distal femur, Proximal tibia | Pain, refusal to bear weight, erythema, warmth, fluctuance, tenderness | Lags 2 weeks behind Destruction of bone, periosteal reaction (lamellated, hair on end), new bone formation | 1. Antibiotics 2. Surgical drainage if required 3. Splintage and rest 4. Supportive treatment for pain and dehydration | |
| Brodie’s abscess | 2-15 years | M>F | Tibia, Femur | Intermittent pain of long duration and tenderness | Radiolucent lesion with a sclerotic margin; elongated serpiginous lucencies | 1. Antibiotics 2. Curettage and bone grafting 3. Wound is loosely closed over a drain | |
| Chronic osteomyelitis | Any | M>F | Tibia, Femur | Flare of acute osteomyelitis, discharging sinus, irregular bone thickening, scars and muscle contractures, bone deformity, pathological fractures | Bone destruction, thickening and sclerosis of surrounding bone, sequestrum, involucrum, cloaca | 1. Antibiotics 2. Debridement (sequestrectomy and saucerization) 3. Dead space management 4. Soft tissue coverage 5. Limb reconstruction | |
| Tubercular osteomyelitis | Tibia, ulna, radius, femur, fibula, humerus | Pain, swelling of bone, warmth, tenderness, soft tissue swelling, cold abscess, sinus, lymph node enlargement | Irregular cavities & areas of destruction, little surrounding sclerosis (honeycomb), soft feathery sequestra, subperiosteal new bone (spina ventosa type), intense sclerosis (secondary infection) | 1. Antitubercular therapy 2. Surgical excision (if refractory, doubtful diagnosis, large abscess) | Sinus: Bluish, undermined margin; serous discharge; anesthesia of surrounding skin | ||
| Osteoid osteoma | 2nd-3rd decades | M:F = 3:1 | Lower extremity long bones | Pain; worse at night, Responds to NSAIDs | Cortical radiolucent nidus <1.5 cm +/- surrounding reactive sclerosis + 1-2 mm peripheral radiolucent zone with marked cortical thickening | 1. NSAIDs 2. Burr down technique 3. CT guided radiofrequency ablation | High levels of COX and PGs in lesion |
| Osteo-blastoma | 10-30 years | M:F = 3:1 | Anywhere | Random pain pattern | Central radiolucent nidus >2 cm, minimal reactive bone reaction | Extended curettage or marginal resection | 40% can have associated aneurysmal bone cyst |
| Conventional osteosarcoma | 2nd decade | M:F = 1.5:1 | Distal femur, Proximal tibia | Progressive pain, Night pain, Tender mass, Limping | Mixed lytic and blastic appearancem cortical destruction, periosteal reaction (codman triangle, sunburst, hair on end), soft tissue mass | 1. Neoadjuvant chemotherapy T-10 protocol (Doxorubicin, Cisplatin, Methotrexate) for 8-12 wks 2. Wide resection and limb reconstruction 3. Adjuvant chemotherapy for 6-12 months (if tumor necrosis <90%; change agents) 4. Amputation (similar outcome like limb salvage) | Associations: RB, Rothmund-Thomson syndrome or Li-fraumeni syndrome |
| Parosteal osteosarcoma | 3rd-4th decade | F>M | Posterior aspect of distal femur, proximal tibia, humerus | Painless mass | Lobulated ossified mass arising from cortex | Wide resection alone | |
| Telangiectatic osteosarcoma | 2nd decade | M>F | Distal femur, Proximal tibia | Progressive pain | Purely lytic, may have ballooned/cystic appearance like ABC | Chemotherapy and wide resection | |
| Ewing’s sarcoma | 1st-3rd decade | M>F | Distal femur, proximal tibia, proximal humerus, fibula | Pain, swelling, low grade fever | Permeative bone destruction, large soft tissue mass, “onion skin” periosteal reaction | 1. Neoadjuvant or Adjuvant chemotherapy or both (VDC-IE protocol) 2. Wide resection +/- adjuvant radiotherapy 3. Radiotherapy | t(11:22) – EWS/FL1 fusion gene; t(21:22); Mic-2 gene; CD99 |
| Non-ossifying fibroma | 1st-2nd decades | M=F | Distal femur, distal tibia, proximal tibia | Asymptomatic | Geographic eccentric lesion, multilobulated appearance with well defined sclerotic margins | 1. Observation 2. Curettage and fixation if large (>50-75% cortex involved) 3. Fractures usually treated nonoperatively | Jaffe-Campanacci syndrome (multiple non-ossifying fibroma with cafe au lait spots) |
| Cortical desmoid | 2nd decade | Male | Posteromedial distal femur | Usually asymptomatic | Erosion of cortex, sclerotic base | Observation | Possibly a reaction to pull of adductor magnus |
| Fibrosarcoma | After 1st decade | M=F | Distal femur, proximal tibia | Pain 20% with pathologic fracture | Purely lytic, destructive | Chemotherapy and wide resection | |
| Unicameral bone cyst (simple) | 1st-2nd decades | M:F = 2:1 | Proximal humerus, proximal femur, proximal tibia | Asymptomatic unless pathologic fracture | Central, lytic, symmetric thinning of cortex, not wider than physis; fallen-leaf sign (small fragment within cavity due to fracture) | 1. Observation (usually regress with skeletal maturity) 2. Aspiration and percutaneous steroid injection (for active lesions, i.e. abuts physis) 3. Curettage and bone grafting (risk of fracture) 4. Fixation and stabilization (pathological fracture proximal femur) | |
| Aneurysmal bone cyst | 1st-2nd decades | M=F | Proximal humerus, distal femur, proximal tibia | Pain and swelling | Eccentric, lytic, expansile radiolucent lesion, thinned cortex, wider than physis; fluid/fluid levels (MRI); persistence of contrast & blush (angiography) | Extended curettage (curopsy) | Secondary ABCs (GCTs, chondroblastoma, osteoblastoma, fibrous dysplasia) |
| Periosteal chondroma | Adults | M=F | Distal femur, proximal humerus, proximal femur | Pain, palpable lump | Superficial erosion of bone cortex with occasional scalloping; popcorn calcification | 1. Curettage 2. Large – resection | |
| En-chondroma | Adults | M=F | Tubular hand bones, proximal humerus, distal tibia | Incidental | Central lobulated areas of stippled calcification (rarely exceed 6 cm), no cortical erosion (except in hands) | 1. Observation with 3-6 monthly serial X-rays for 1-2 yrs 2. Curettage if symptomatic | Ollier disease (multiple enchondromatosis – 20 to 30% malignant transformation – secondary central chondrosarcoma) Maffucci syndrome (multiple enchondromatosis with soft tissue hemangiomas – >50-100% malignant transformation) |
| Osteo-chondroma | 2nd-3rd decades | M>F | Femur, humerus | Mass, Pain (adventitious bursa, fracture, compression) | Pedunculated or sessile bone lesion that communicates with intramedullary canal of host bone Lesion has overlying cartilage cap | 1. Observation (asymptomatic >2 cm cartilage cap) 2. Resection for pain | Malignant transformation – secondary peripheral chondrosarcoma (<1%; pain without pressure effects) Multiple Hereditary Exostoses/Diaphyseal aclasia (MHE) – EXT1 or 2 mutation (4% malignant transformation) |
| Chondro- myxoid fibroma | 10-30 | M>F | Proximal tibia | Pain | Eccentric lytic lesion (bubbly), parallel to long axis of bone, little or no periosteal/soft tissue reaction | Extended curettage | Important to distinguish from chondrosarcoma |
| Conventional chondro-sarcoma | 5th-7th decades | M>F | Pelvis, proximal femur, proximal humerus | Progressive pain | Punctate (honeycomb or popcorn) calcification, cortical erosion, grow along intramedullary canal (least resistance), soft tissue mass | 1. Wide resection and reconstruction for high grade (mean 11.8 cm intramedullary extent i.e. large, bone expansion, periostitis, soft tissue mass) 2. Extended curettage or RFA for low grade (mean 5.5 cm intramedullary extent i.e. small) | No role for chemotherapy and radiation IDH1 or 2 mutation (60%) |
| De- differentiated chondro-sarcoma | 5th-8th decades | M>F | Pelvis, proximal femur, proximal humerus | Progressive pain, patholgical fracture (30%) | Aggressive radiolucent lesion adjacent to otherwise typical chondrosarcoma | Chemotherapy and wide resection | Poor prognosis |
| Giant cell tumor | 20-40 | F>M | Distal femur, proximal tibia, distal radius, proximal humerus | Pain, Pathologic fracture (10-30%) | Eccentric, expansile, lobulated lytic lesion with narrow zone of transition, abuts subchondral bone; may exhibit cortical erosion with soft tissue extension; little or no periosteal reaction/matrix calcification | 1. Campanacci Stage 1 and 2: extended intralesional curettage (phenol, bone cement, liquid nitrogen) 2. Stage 3: Thorough curettage or en-bloc resection (if residual bone stock inadequate) 3. Resection of pulmonary mets. 4. Bisphosphonate 5. Denosumab | 3% incidence of benign pulmonary mets.; Malignant transformation <1%; Secondary ABCs 20%; Metaphyseal in skeletally immature patients |
| Metastases | 5th-8th | M=F | Proximal femur, Proximal humerus | Pain, swelling, pathological fracture, symptoms of hypercalcemia, symptoms referable to primary lesion | Blastic- Prostate Mixed – Breast, Lung Lytic – kidney | 1. Bisphosphonates 2. RFA 3. Radiation for symptomatic bone lesions 4. Surgery for impending or actual pathologic fractures |

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.