Normal puerperium has been already discussed earlier here.
A) Immediately after labor within 1 hour
- Blood pressure and heart rate atleast every 15 minutes
- Monitor amount of vaginal bleeding
- Palpate fundus to ensure amount adequate contractions (if relaxed – massage uterus to enhance oxytocin release)
B) 1st several hours
1. Early ambulation: Out of bed (OOB) within a few hours after delivery –
- Decreases puerperal venous thrombosis and pulmonary embolism
- Decreases bladder complications
- Decreases constipation
- Facilitates uterine drainage and hastens involution
2. Care of vulva: Taught to cleanse and wipe vulva from front to back
3. If Episiotomy/Laceration repair:
- Ice pack for 1st several hours to reduce edema and pain
- At 24 hour postpartum – moist heat (warm sitz baths) can decrease local discomfort
- Episiotomy incision is typically well healed and asymptomatic by 3 weeks
- Inspection of the site daily
4. Bladder function: Ensure that postpartum woman has voided within 4-6 hours of delivery; if not –
- Indwelling catheter may be necessary or if residual urine >60 ml
- Bladder sensation and capability to empty may be diminished due to anesthesia
- Consider a hematoma of genital tract (reflex pain) as possible etiology
- A prolonged second stage of labor or operative delivery may traumatize the base of the bladder and interfere with normal voiding and is significantly associated with protracted urinary retention beyond the third postpartum day.
C) 1st Few days
1. Bowel function:
- The mild ileus that follows delivery, together with perineal discomfort and postpartum fluid loss by other routes, predisposes to constipation during the puerperium.
- Encourage early ambulation and feeding
- Ask the patient about flatus
- If needed, mild laxatives at bedtime stimulates bowel movement by next morning
- If not improved – rectal enemas may be given
- Hemorrhoids may be increased due to prolonged 2nd stage of labor pushing efforts – usually repsonds to conservative treatment with compresses, suppositories containing corticosteroids, local anesthetic sprays or emollients and sitz baths
2. If 4° laceration:
- Fecal incontinence may result, even with correct surgical repair due to injury to innervation of pelvic floor musculature
- Stool softener and low residue diet to reduce straining and risk of fistula formation
- Avoid enemas or suppositories which can disrupt the repair
3. Discomfort/pain management:
- Afterpains:
- Uterine massage
- Expulsion of clot
- NSAIDs (Ibuprofen)
- Antispasmodics
- Episiotomy/laceration pain: NSAIDs or Narcotic medication
- Breast engorgement: Well-fitted brassiere; NSAIDs
- Postspinal puncture headache:
- Caffeine; blood patch
- Constipation and urinary retention
4. Diet:
- Permitted to eat and dring normal diet of choice – if uncomplicated vaginal delivery
- Those with uncomplicated Cesarean section can be given clear liquids and regular diet as tolerated
- Continue iron and calcium supplementation during puerperium
- Recommended calorie intake: 500 kcal/day more than usual
5. Immunization:
- Anti-D gamma globulin: 300 mcg within 72 hours to non-isoimmunized D negative mothers with D positive baby
- Three hundred grams will neutralize approximately 30 mL of whole fetal blood (or 15 mL of Rh+ fetal red blood cells).
- Rho (D) immunoglobulin is administered after abortion without qualifications or after delivery to women who meet all of the following criteria: (1) The mother must be Rho (D)-negative without Rh antibodies, (2) the baby must be Rh (D)+ or Rh (D)-/Du-positive, and (3) the cord blood must be Coombs-negative. If these criteria are met, a 1:1000 dilution of Rho (D) immunoglobulin is cross-matched to the mother’s red cells to ensure compatibility, and 1 mL (300 μg) is given intramuscularly to the mother within 72 hours after delivery. If the 72-hour interval has been exceeded, it is advisable to give the immunoglobulin rather than withhold it because it may still protect against sensitization 14–28 days after delivery, and the time required to mount a response varies among cases.
- Rubella vaccine: if not immune previously; mandatory postponement of pregnancy ≥2 months
- TT booster at time of discharge
D) Discharge
If Normal Vaginal Delivery: after 1 day, along with education and instructions
- Follow up at 4-6 weeks for postpartum examination
If Cesarean section without complications: After 3-4 days post-delivery
- Follow up at 2 weeks to check incision and 4-6 weeks for postpartum examination
Instructions: return if –
- Fever >37 °c
- Excessive vaginal bleeding – soaking a pad an hour (possible retained placenta)
- Lower extremity pain and/or swelling (suspicious for DVT)
- Shortness of breath (suspicious for pulmonary embolism)
- Chest pain (can occur with pulmonary embolism)
Postpartum examination:
- Record patient’s weight and blood pressure
- Breast examination for abnormalities of nipples or lactation or detection of mass
- Complete rectovaginal examination
- Examination of episiotomy incision and repaired lacerations
- If pelvic organ prolapse detected – Hysterectomy or vaginal repair is best postponed for at least 3 months after delivery to allow maximal restoration of the pelvic supporting structures
E) Postpartum coitus
- After 6 weeks, coitus may be resumed based on patient’s desire and comfort
- Dangers of premature intercourse:
- Pain due to continued uterine involution and healing of laceration/episiotomy scars
- Increased likeliood of hemorrhage and infection
- A water-soluble lubricant or vaginal estrogen cream is especially helpful in lactating amenorrheic mothers in whom vaginal atrophy occurs, usually because of low circulating estrogen levels.
F) Contraception
Don’t wait until 1st menstruation to begin contraception – ovulation may come before 1st menstruation
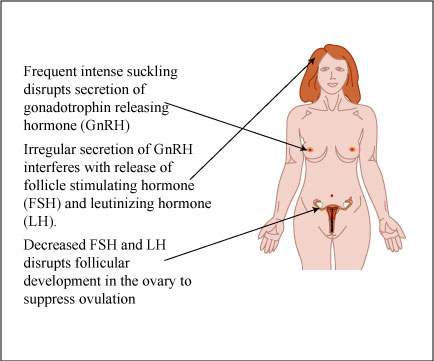
- Lactational amenorrhea method (LAM):
- Exclusive breastfeeding to prevent ovulation – 98% effective for upto 6 months if –
- mother is not menstruating
- mother is nursing > 2-3 times/night and > 4 hrly during day
- baby is <6 months old
- If no breastfeeding – menstruation returns by 6th week (40%) to 12th week (80%)
- Non-breastfeeding mother should use contraceptive in 3rd postpartum week and lactating mother in 3rd postpartum month
- Exclusive breastfeeding to prevent ovulation – 98% effective for upto 6 months if –
- Tubal ligation:
- At time of cesarean section
- Within 48 hours postpartum after vaginal delivery
- 6-8 weeks postpartum is preferred because it allows time to:
- ensure that infant is healthy
- understand implications of permanent sterilization
- decrease feeling of guilt or regret
- Long-term complications, such as the posttubal syndrome (irregular menses and increased menstrual pain) have been reported in some 10–15% of women
- OCPs in postpartum:
- Oral contraception should be deferred until 6 weeks postpartum because of concerns about the postpartum hypercoagulable state
- Combined OCPs decrease amount of breast milk and very small quantities of hormones are excreted in milk
- Progestin only OCPs (95% effective): no reduction in amount of breast milk; need to take it same time everyday
- Depo-medroxyprogesterone: 99% effective; 150 mg i.m every 3 months
- The level of progestin in depot medroxyprogesterone acetate raises the seizure threshold and is the contraceptive of choice for women with seizure disorder
- Concerns related to prolonged amenorrhea, prolonged return to fertility, the inconvenience of unscheduled bleeding, weight gain, skin changes, and reversible bone density reduction and lipid metabolism changes are potential reasons for discontinuation
- Levonorgestrel implants: Immediately postpartum or by 6 weeks
- IUD:
- Interval insertion: Placed at 1st postpartum visit
- May be placed as early as immediately postpartum (higher risk of expulsion)
- The main side effects include <1% risk of pelvic infection in the first 2 weeks after insertion, uterine perforation (<1%), expulsion (<3%), and abnormal uterine bleeding.
- The risk of uterine perforation during IUD insertion is higher in lactating women, probably because of the accelerated rate of uterine involution. Of note, the risk of expulsion is not increased in these lactating women. Uterine perforation is highest when insertion is performed in the first 1–8 weeks after delivery
A very good and informative slides
excellent presentation which is quite useful and detailed
very very use full this slide