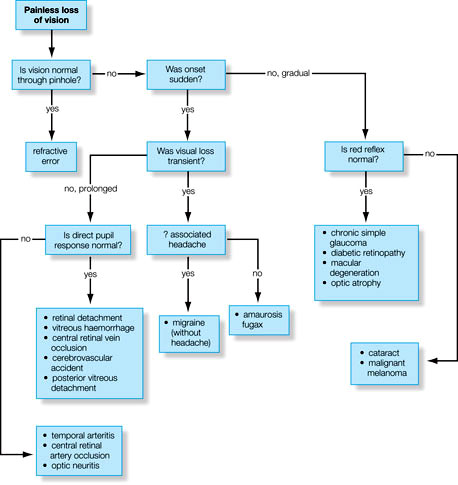
Diagnosis of the etiology of vision loss requires a step-wise systematic approach. The vision loss may be sudden or gradual, painful or painless, unilateral or bilateral, etc. One needs to take a detailed ocular history and examination.
Step 1: Sudden or gradual vision loss?
a. Sudden: vascular occlusion (e.g., AION, CRAO, CRVO) or bleeding (e.g., vitreous hemorrhage, “wet” macular degeneration).
b. Gradual: degenerations or depositions (e.g., cataract, macular dystrophies or “dry” macular degeneration, corneal dystrophies).
Step 2: Associated with pain?
- Associated pain is a common finding in anterior ocular processes (e.g., keratitis, anterior uveitis)
- Other painful conditions: orbital disease, optic neuritis, and giant cell arteritis
Step 3: Transient or persistent vision loss?
a. Transient: temporary/subcritical vascular insufficiency (e.g., giant cell arteritis, amaurosis fugax, vertebrobasilar
artery insufficiency) or papilledema
b. Persistent: structural or irreversible damage (e.g., vitreous hemorrhage, macular degeneration).
Step 4: Unilateral or Bilateral vision loss?
a. Unilateral: a local cause or lesion anterior to optic chiasma
b. Bilateral: a more widespread or systemic process or lesion posterior to optic chiasma
Step 5: Blurred, dimmed or distorted vision (What)?
a. Blurring or dimming: pathology anywhere in the visual pathway from cornea to cortex; common problems include refractive error, cataract, and macular disease.
b. Distortion: macular pathology, high refractive error (high ametropia/astigmatism) or other ocular disease.
Step 6: Where is the vision loss?
a. Superior or inferior hemispheric field loss (Altitudinal): corresponding inferior or superior vascular event involving the retina (e.g., retinal vein occlusion) or optic disc (e.g., segmental AION)
b. Peripheral field loss: retinal detachment (usually rapidly evolving from far periphery), optic nerve disease, chiasmal compression (typically bitemporal loss), or cortical pathology (homonymous hemianopic defects)
c. Central blurring of vision: diseases of the macula (positive scotoma: a “seen” spot) or optic nerve (negative scotoma: an unseen defect).
Step 7: When is the vision loss ?
Glare: from headlights or bright sunlight due to posterior subcapsular lens opacities
Further investigations is based upon the disease suspected from history and ophthalmic examination.
Adapted from Oxford Handbook of Ophthalmology