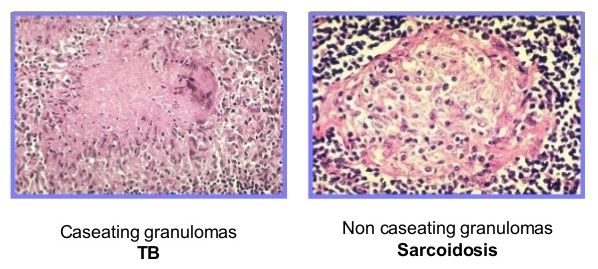
Sarcoidosis and tuberculosis are both granulomatous disease with similar constitutional symptoms, respiratory symptoms and multiple organ involvement with hilar and mediastinal lymph node involvement. Hence, the diagnosis of one from the other may pose significant difficulties.
Sarcoidosis vs Tuberculosis (TB)
IFN-gamma release assays (IGRA)Tuberculosis can be reliably excluded if both Mantoux test and IGRA is negative.
| Features | Sarcoidosis | Tuberculosis |
| Epidemiology | African American and American populations
Scandinavia |
TB endemic regions – Subsaharan Africa, Asia
Homeless, prison populations, drug abuse |
| Increased susceptibility | HLA association
Family history (5 fold risk) |
Defects in cell mediated immunity (CMI), HIV |
| Clinical differences | ||
| Skin lesions | Common | Rare (lupus vulgaris) |
| Lupus pernio | Diagnostic | None |
| Erythema nodosum | Common | Rare |
| Eye disease | Common | Rare |
| Pleural disease | Very rare | Common |
| Cranial nerve VII palsy | Common | Rare |
| Pattern of organ involvement | Uveal tract, salivary and lacrimal glands, heart and skeletal muscles, liver and spleen and small bones of hand and feet are commonly involved in sarcoidosis but are rarely seen in tuberculosis. | Adrenal glands may be involved in caseating tuberculosis but almost never in sarcoidosis.
Involvement of small intestine is common in TB but rare in sarcoidosis. |
| Marked constitutional symptoms like night sweats and weight loss | 12% | More suggestive of tuberculosis |
| Lab investigations | ||
| Hypercalcemia | Can occur | Very rare |
| Serum ACE | Elevated in 87% | Elevated in 4% |
| Mantoux test | Anergic
Negative in 90% |
Positive in 65-94% |
| Kveim-Siltzbach test | Positive in 60% | Negative |
| Bronchoalveolar lavage (BAL) lymphocytes
BAL CD4/CD8 ration > 3.5 |
Very common | Common |
| Histology/microscopy | Defined non-caseating granuloma | Caseating granulomas ‘Acid fast’ positive bacilli |
| Isolation of mycobacterium tuberculosis | None or incidence similar to control groups | Positive |
| Radiological differences | ||
| Hilar and mediastinal lymphadenopathy | Symmetrical and Bilateral | Asymmetrical and usually unilateral |
| Other | Diffuse or micronodular interstitial infiltrates
Upper lobe fibrosis Rarely diffuse alveolitis or cavitating masses |
Necrosis common
Upper-lobe infiltrates with cavitation, tree-in-bud, macro-nodular infiltrates. Cavitation is more common in TB. |
| Treatment | ||
| Immunosuppresives like steroids | Antitubercular therapy including Isoniazid, Rifampicin, Ethambutol, Pyarzinamide | |
References:
- Sarcoidosis edited by Donald N Mitchell, Athol Wells, Stephen G Spiro, David R Moller
- Oxford Textbook of Medicine Vol. 1
- Challenging cases in pulmonology by Massoud Mahmoudi