Approach the patient with 9 Ps.
0-10 minutes (Possibility of Success): Anticipating difficult airway
Mnemonic: LEMON approach
1. Look externally: Remember “BONES“
- Beard
- Obesity
- No teeth
- Elderly
- Sleep apnea/Snoring
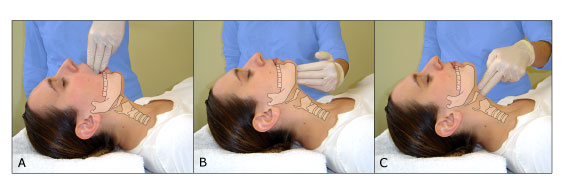
2. Evaluate 3-3-2 rule: Ideal dimensions for visualization of larynx
- 3 fingers in mouth: adequate mouth opening
- 3 fingers under the chin (mentum to hyoid bone): mandible large enough to accomodate tongue
- 2 fingers at top of neck (hyoid bone to thyroid cartilage): adequate neck length and laryngeal position
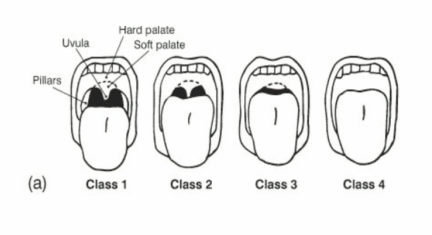
3. Mallampati: Predict ability of patient’s mouth to accomodate both laryngoscope and ET tube – class III and IV indicate limited oral access
- Class I: faucial pillars, soft palate, and uvula visualized
- Class II: faucial pillars and soft palate visualized, but the uvula is masked by the base of the tongue
- Class III: only the base of the uvula can be visualized.
- Class IV: none of the three structures can be visulaized
4. Obstruction of upper airway: Infections, tumors, foreign body, etc.
5. Neck mobility
0-10 minutes: Preparation
Mnemonic: SOAP ME
1. Suction
2. Oxygen (mask and BVM ventilation)
3. Airway equipment:
- Laryngoscopes: Atleast 2 functioning handles and various sized blades
- ET tube: Chosen size and one size smaller ETT must be available and ET cuff must be tested
- Adult male: 7.5-8
- Adult female: 7-7.5
- Children: 4 + (age in years/4)
4. Pharmacy:
- Patent IV line
- Specific RSI medications: Proper dosing, Sequence of administration, Agents drawn up and labelled
5. Monitoring Equipment: Blood pressure and Pulse oximetry (ETCO2 if available)
0-5 minutes: Preoxygenation
- “Nitrogen washout” with 100% oxygen for 5 minutes – replace room air (80% nitrogen + 20% oxygen) with 100% oxygen in lungs to create oxygen reservoir
0-3 minutes: Pretreatment
Mnemonic: LOAD
- Lidocaine
- Opioid (fentanyl)
- Atropine
- Defasciculation (Pancuronium, Vecuronium)
Zero minutes: Paralysis
1. Induction:
- Choice: Etomidate
- Hypotensive, Hypovolemic and Bronchospastic patients: Ketamine
- Others: Thiopental, Methohexital, Midazolam, Propofol
2. NM Blockade:
a. Depolarizing agent:
- Succinylcholine: Onset: 45-60 seconds; Duration: 6-12 minutes
b. Non-depolarizing agent:
- Rocuronium: Onset: 50-70 seconds; Duration: 30-60 minutes
- Vecuronium: Onset: 90-120 seconds; Duration: 60-75 minutes
- Pancuronium: Onset: 100-150 seconds; Duration: 120-150 minutes
For the dosage and brief pharmacology: https://med.umkc.edu/docs/em/Intubation_Chart.pdf
0 + 20-30 seconds: Protection and Positioning
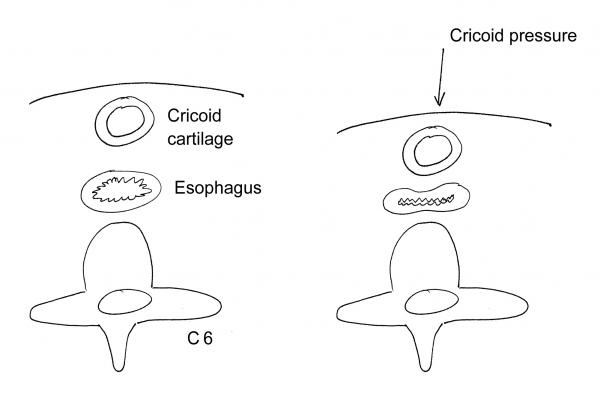
Sellick’s maneuver (Cricoid pressure) by assistant:
- Start: After patient begins to lose consciousness (prevent patient discomfort and vomiting)
- Application: 10lbs pressure to cricoid to compress esophagus and prevent regurgitation of gastric contents
- End: After ETT is placed, position verified and cuff inflated
Positioning:
- Sniffing position: Flexion of neck on body and Extension of head on neck to align 3 axes (oral, phayngeal and laryngeal)
- C-spine injury suspected: Use neutral position
0 + 45 seconds: Placement
a. Laryngoscope
- Confirm complete paralysis: check for flaccidity of mandible
- Open mouth with right hand
- Hold larygoscope in left hand
- Insert laryngoscope into the right side of the patient
- Tongue is displaced to the left
- Curved (Macintosh) blade is slid into valeculla; Straight (Miller) blade is positioned below epiglottis
- Laryngoscope handle is advanced along the axis of the blade at an angle of 45° to the patient’s body.
- If laryngeal apparatus not vissible: Apply “BURP” maneuver – Backward, Upward and Right Pressure on thyroid cartilage
b. ET tube
- Insert ETT tube with right hand until cuff is 2-3 cm below vocal cords (23 cm marker on corner of mouth in adult male and 21 cm in adult female)
- Remove stylet
- Inflate cuff
0 + 45 seconds: Proof of correct ETT placement
a. Clinical:
- Laryngoscopist observing ETT pass through vocal cords
- Clear and equal breath sounds over both lung fields
- Absence of breath sounds over epigastrium
- Symmetrical chest rise during ventilation
- Fogging of ETT during ventilation
b. Pulse oximetry (not a primary indicator): drop in SpO2 may indicate esophageal intubation
c. ETCO2 detection:
- “Normal square waveforms” will not be detectable in capnograph if esophageal intubation has occured
- Color change from purple to yellow will be absent in colorimetric ETCO2 detector if esophageal intubation has occured
d. Suction apparatus:
- ET tube in esophagus (collapsible): resistance with attempt to suction
- ET tube in trachea (non-collapsible due to cartilage rigns): free flow of air with attempt to suction
0 + 1 minute: Post-intubation management
- Secure tube in place
- Monitor vitals frequently
- Bradycardia may suggest hypoxia due to esophageal intubation
- Hypertension suggests inadequate sedation
- Hypotension may suggest tension pneumothorax, decreased venous return, cardiac cause or induction agent
- Configure mechanical ventilator
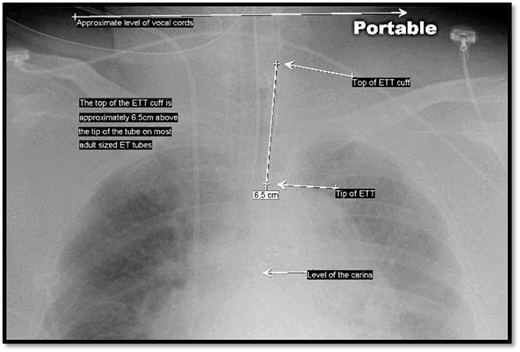
- CXR to assess ET tube position and condition of patient’s lungs (proper tube depth is 2-3 cm above carina)
- Long-term sedation and paralysis:
- Diazepam 0.2 mg/kg or Lorazepam 0.05-0.1 mg/kg (may be repeated for any signs of awareness)
- Pancuronium 0.1 mg/kg or Vecuronium 0.1 mg/kg (1/3rd of intial dose may be repeated after 45-60 minutes if motor activity is detected)
LIVES Mnemonic for Tracheal Intubation
| Equipment | Action | |
|---|---|---|
| L | Laryngoscope | Left-handed laryngoscopy |
| I | Intubation tube | Intubation and insufflation of the cuff using a syringe |
| V | Ventilatory device | Ventilation |
| E | End-tidal CO2 monitor | Evaluation of tube position with monitor and by auscultation |
| S | SaO2 monitor | Secure with tie and monitor oxygen saturations |
Watch the whole thing
References:
- An Introduction to Clinical Emergency Medicine by S.V. Mahadevan and Gus M. Garmel
- BJA: British Journal of Anaesthesia, Volume 118, Issue 2, February 2017, Pages 270–271, https://doi.org/10.1093/bja/aew459