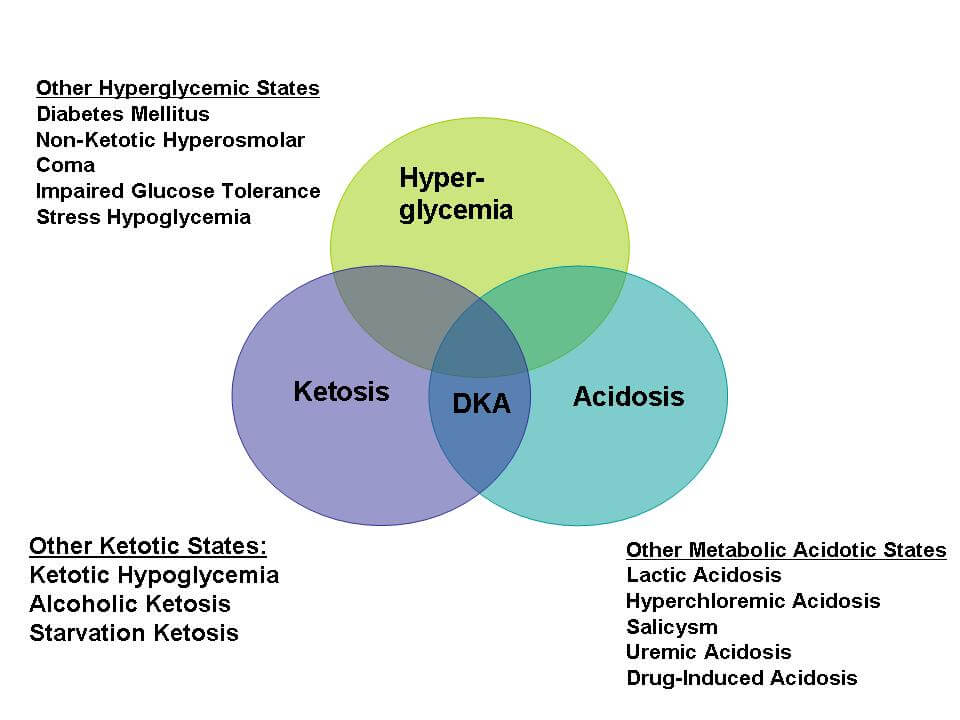
Diagnostic criteria for DKA
a. Plasma glucose (mg/dl): >250
b. Arterial pH:
- 7.25 to 7.3: mild DKA
- 7 to 7.24: moderate DKA
- <7: severe DKA
c. Serum bicarbonate (mEq/L):
- 15 to 18: mild DKA
- 10 to 15: moderate DKA
- <10: severe DKA
d. Urine and serum ketones (nitroprusside reaction): Positive
e. Effective serum osmolality (mOsm/kg): Variable
- Calculated osmolality = 2 X [Na+] + [Glucose]/18 + [BUN]/2.8
- Effective osmolality = 2 X [Na+] + [Glucose]/18
Sodium concentration is multiplied by a factor of 2 to include the chloride and bicarbonate that are present to maintain electroneutrality. Concentrations of urea and glucose are measured in mg/dl and must be converted to millimoles per liter by the conversion factor of 2.8 for BUN and 18 for glucose.
f. Anion gap (mEq/L): [Na+] – [Cl-] – [HCO3-]
- >10: mild DKA
- >12: moderate and severe DKA
g. Mental status:
- Alert: mild DKA
- Alert/drowsy: moderate DKA
- Stupor/coma: severe DKA
The most widely used diagnostic criteria for DKA are plasma glucose >250 mg/dL, arterial pH <7.3, and presence of ketonemia and/or ketonuria.
Average Fluid and Electrolyte Deficit in DKA
- Free water: 100 ml/kg
- Sodium: 7-10 mEq/kg
- Potassium: 3-5 mEq/kg
- Chloride: 3-5 mmol/kg
- Phosphorous: 1 mmol/kg
Precipitating factors in DKA
Mnemonic: 5 I
- Infections (30-50%): Pneumonia, UTI, Sepsis, Gastroenteritis
- Inadequate insulin (20-40%): Non-compliance, Insulin pump failure
- Ischemia or Infarction:
- Heart: Myocardial (3-6%) – often “silent”
- Brain: Stroke
- Intestine: Mesenteric ischemia
- Lungs: Acute pulmonary embolism
- Intoxication (Alcohol)
- Illness – Acute pancreatitis, Severe burns, Thyrotoxicosis
Prinicples of Management of DKA
Use your “HEAD” backwards
a. Dehydration management
b. Anion gap
c. Electrolytes
d. Hyperglycemia
Important steps to follow in early stage of DKA management
Mnemonic: ACTRAPID (Stepwise)
a. Airway, Breathing and Circulation and Analysis: Stabilize and Send blood for metabolic profile before initiation of fluids)
b. Commence fluid resuscitation:
- Initial fluid therapy: 0.9% NaCl (NS) 1 L/hour (15-20 ml/kg) in 1st hour and until resolution of severe volume depletion (indicated by orthostatic hypotension or supine hypotension with dry mucous membranes and poor skin turgor)
- Calculate corrected sodium: Add 1.6 to 2.4 (average 2) mEq/L sodium for 100 mg/dl plasma glucose above 100 mg/dl
- Hyponatremic patients: NS @ 250-500 ml/hr (4-14 ml/kg) and when plasma glucose reaches 200 mg/dl, change fluid therapy to 5% Dextrose with 1/2 NS @ 150-250 ml/hr
- Eunatremic and hypernatremic patients: 1/2 NS @ 250-500 ml/hr and when plasma glucose reaches 200 mg/dl, change fluid therapy to 5% Dextrose with 1/2 NS @ 150-250 ml/hr
c. Treat potassium:
- Aim: K+ 3.3 to 5.3 mEq/L
- Withold insulin therapy until K+ >3.3 mEq/L or stop insulin whenever K+ <3.3 mEq/L
- Whenever K+ <5.3 mEq/L and adequate urine output of >50 ml/hour, 20 to 30 units (mEq) of K+ should be added to each liter of infusion fluid
- If K+ >5.3 mEq/L, replacement is not needed (but K+ should be checked 2 hourly)
d. Replace Insulin:
- Initiate insulin only after giving 1 L NS over 1 hour and correcting K+ to >3.3 mEq/L
- Bolus then continuous infusion (0.1 U/kg regular insulin followed by continuous infusion of 0.1 U/kg/hr) OR Continuous infusion (0.14 U/kg/hr)
- If blood glucose does not fall by 10% or 50 mg/dl in the first hour of insulin infusion: an additional bolus (0.1 Unit/kg or 0.14 Unit/kg, respectively) may be given and the infusion then continued at the previous rate.
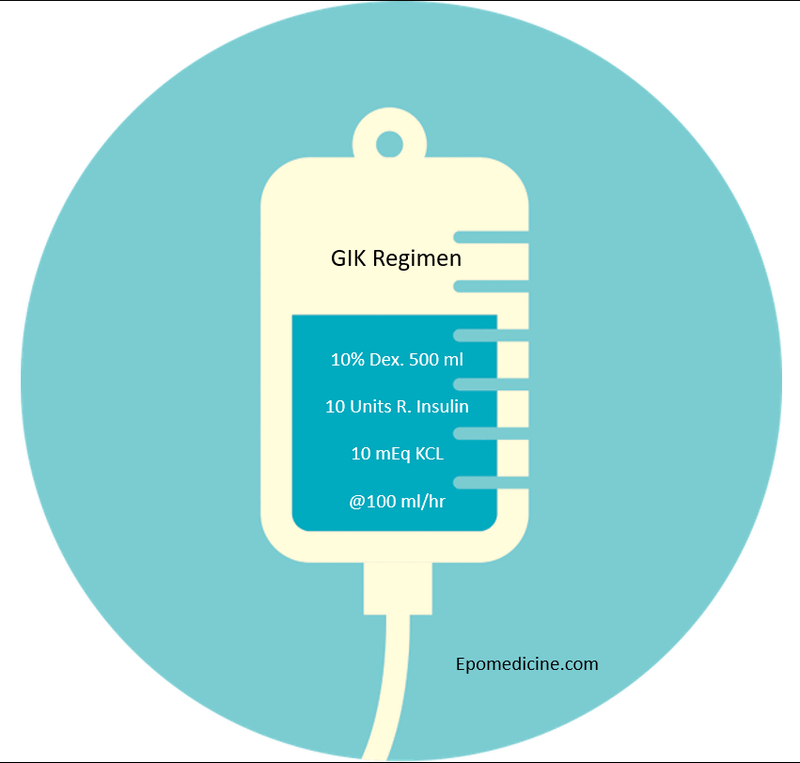
- Once plasma glucose reaches 200 to 250 mg/dL: insulin rate may be decreased by half, or to a rate of 0.02 to 0.05 U/kg/hour. In addition, dextrose should be added to the maintenance IV fluids at this point to prevent potential hypoglycemia.
- The rate of insulin infusion (or the dextrose concentration) should then be adjusted to maintain a plasma glucose level of between 150 and 200 mg/dL.
In patients with mild to moderate DKA that is not complicated by acute MI, congestive heart failure, end-stage renal or hepatic failure, steroid use or pregnancy, alternative subcutaneous regimen can be used. Dosing regimens consist of 0.2 Unit/kg initially, followed by 0.1 Unit/kg every 1 hour or 0.3 Units/kg initially, followed by 0.2 Unit/kg every 2 hours until blood glucose is less than 250 mg/dL. At this point, insulin should be decreased to 0.05 to 0.1 Unit/kg, respectively, every 1 to 2 hours until the DKA is resolved.
Acidosis management:
In adult patients with pH <6.9, it is recommended that 100 mmol sodium bicarbonate in 400 mL sterile water (an isotonic solution) with 20 mEq KCl be administered at a rate of 200 mL/hour for 2 hours until pH >7.0.
For monitoring of treatment, venous pH is sufficient and should be checked at least each hour in this setting. Treatment should be repeated every 2 hours until pH >7.0.
Prevent complications:
Complications usually result from the pathological process of DKA or too fast a reversal of the hyperglycaemia/osmolarity. Complications can include dehydration, hypovolaemia, hypotension, electrolyte abnormalities, cardiac arrhythmias, cardiac arrest and cerebral oedema.
Investigate (Monitor) therapy:
Subsequent to initial laboratory evaluation:
- Serum glucose and electrolytes hourly
- Calcium, magnesium and phosphate 2 hourly
- BUN, creatinine and ketones 2-6 hourly
Management and monitoring should continue until DKA resoultion indicated by:
- Plasma glucose <200 mg/dl (At this point, insulin can be decreased by 50%)
- Serum bicarbonate >10 mEq/L
- Venous pH >7.3
- Anion gap <10
Discharge:
The aim is to discharge the patient with sufficient education to prevent re-admission with DKA in the future.
Reference:
https://online.epocrates.com/diseases/16241/Diabetic-ketoacidosis/Treatment-Approach

Wonderful strategy to get success in neet PG
My rating to epomedicine is 10 out of 10.
Very comprehensive and enjoyable notes, I enjoyed