Before we start to develop our understanding of the drug eruptions. Let’s first lay down the foundation by clearing some basic concepts.
- What is an Allergy?
- What is meant by an adverse drug reaction?
- What is the diversity of allergic reactions due to drugs?
Allergy
This is a hypersensitivity disorder of the body’s immune system; so, it starts producing a damaging inflammatory reaction to the substances against which a healthy immune system is not supposed to respond or response is so intense that it produces marked collateral damage.
Adverse drug reaction
These are those undesirable reactions that accompany the desirable effects of a drug. They include; drug side effects, drug-drug interaction, drug toxicity & associated illness, and drug allergy.
Diversity of drug-related allergy
The inflammatory reaction which is initiated by a hypersensitive immune system can produce damage to any organ, e.g. acute tubular necrosis in the kidney or drug eruptions in the skin.
What are Drug Eruptions?
Adverse inflammatory reactions involving the skin and its appendages or mucous membrane produced by drugs.
What Causes Drug Eruptions?
- Immunologically mediated reactions
- Nonimmunologically mediated reactions
1. Immunological mechanism
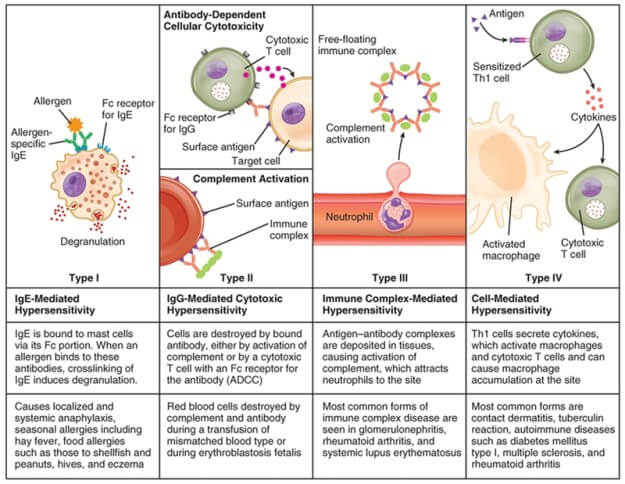
a. Type I reaction
- IgE-mediated mast cell degranulation
b. Type II reaction
- Cytotoxic; cellular lysis induced by the direct binding of the antibody to cell surface antigens.
c. Type III reaction
- Immune complex deposition in tissues which then recruits inflammatory cells and release of mediators which then cause damage
d. Type IV reaction
- Delayed, CD8+ T cell-mediated
2. Nonimmunological mediated reactions
a. Predictable mechanism
- Pharmacological side effect: Hair fall due to chemotherapy
- The secondary pharmacological side effect: Thrush while taking antibiotics
- Drug toxicity: Purpura with anticoagulant overdose
b. Unpredictable mechanism
- Idiosyncratic:
- Anaphylactic reaction after radiocontrast media
- Rash in Infectious mononucleosis patient on Ampicillin
- Drug-induced lupus (DLE) due to Procainamide
The spectrum of Drug Eruptions
The spectrum of the disease range from a Clinically mild and unnoticed rash to a severe cutaneous adverse reaction (SCARs) that may be life-threatening.
Morphology of Drug Eruption Lesion and Commonly Associated drugs
Drug eruption shows a wide range of morphological lesions. Anything you can think of, anything you have seen, and something that you don’t even think of can be due to drugs.
While going through drug eruptions it is important to appreciate the morphology and physical features of drug eruptions and drugs commonly associated.
Acneiform Eruption
- Comedones are absent, that’s how it’s different from actual acne.
- Corticosteroids, OCPs, Phenobarbitone
Bullous eruption
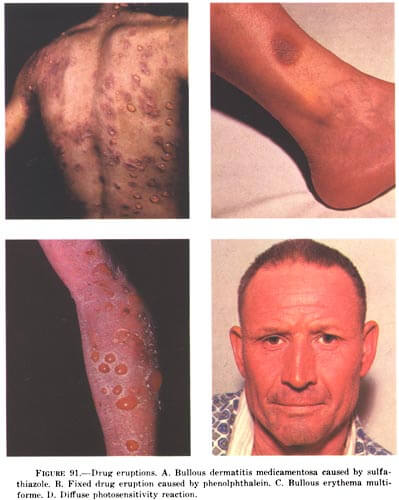
- Several types. Tense, thick-walled bullae often seen in barbiturate overdosage.
Eczematous
- Due to contact with various drugs or chemicals or exacerbation of existing contact dermatitis on systemic administration of offending agents such as penicillin, sulphonamides, neomycin, and nitrofurazone.
Acral erythema
- Erythrodysesthesia
- Reddening, swelling, numbness, and desquamation (skin sloughing or peeling) of acral body parts (hands & feet)
- Chemotherapy related drugs cisplatin, cyclophosphamide, doxorubicin, fluorouracil, MTX
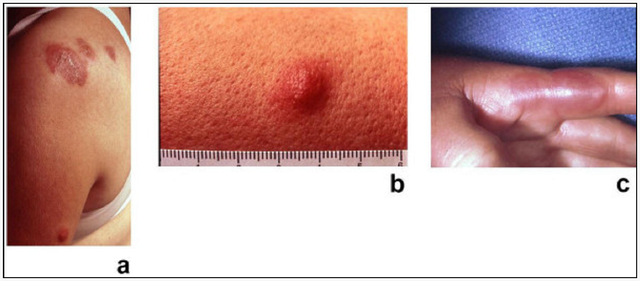
Erythema nodosum
- Type IV hypersensitivity reaction
- Characterized by tender, red, subcutaneous nodules that typically appear in the anterior aspect of the legs, don’t ulcerate.
- Medications, especially oral contraceptives and sulfonamides
Fixed drug eruptions
- Characteristically recurs in the same site each time the same or chemically related drug administered.
- Lesions sharply demarcated round or oval plaques of erythema and edema becoming dusky, violaceous, or brown. Sometime surmounted by large bulla.
- Common sites of the lesion are Hands, genitalia, oral mucosa & heals.
- Common drugs; Sulphonamides, Trimethoprim, Tetracyclines, Paracetamol
Lichenoid eruption
- Lichen planus like eruption, but oral lesions are absent and lesions have scales
- PAS, Streptomycin, INAH, Phenothiazines
Lupus-like syndrome
- Lesion is like systemic lupus erythematous cutaneous manifestation; malar rash, discoid rash.
- ANA factor often positive but rarely involve kidney often settle once offending drug is withdrawn
- Commonly associated drugs; hydralazine, procainamide, and minocycline. Beta-blockers, chlorpromazine, cimetidine, clonidine, estrogens, isoniazid
Morbilliform or exanthematous eruption
- Symmetrical distribution mainly on the trunk
- Initially erythematous blanching macules and papules, later on, no blanching petechiae like lesions
- ACE inhibitors, Allopurinol, Ampicillin, Anticonvulsants
Serum sickness and serum sickness-like reaction
- Type 3 hypersensitivity reaction
- No immune complex found in serum sickness-like reaction but present in serum sickness
- Although both have the same presentation fever, Rash (wheal with central clearing common on the trunk and extremities), joint pain & lymphadenopathy.
Acute febrile neutrophilic dermatosis
- Sweet syndrome
- Characterized by a sudden onset of fever and painful rash on the arms, legs, trunk, face, or neck
- All-trans -retinoic acid, celecoxib, granulocyte colony-stimulating factor, nitrofurantoin, oral contraceptives
Urticaria
- Type 1 hypersensitivity reaction
- Severity varies
- Mild: wheals and hive
- Moderate: angioedema involves swelling of the tongue, lips &mucosa
- Severe: the form is anaphylaxis in which pt. is in shock
- ACE inhibitors, Aspirin/NSAIDs, Blood products, Cephalosporins, Opioids, PPI
Vasculitis
- Type 3 hypersensitivity reaction
- Nonblanchable purpura
- Tetracycline, Aspirin/NSAIDs, Levofloxacin, PPIs, Sulfonamides
Erythroderma
- Intense inflammatory reactions cause widespread reddening of skin > 90% body surface area is involved
- This is due to marked vasodilation due to the massive release of inflammatory mediators
- Allopurinol, anticonvulsants, aspirin, barbiturates, captopril, carbamazepine
Erythema multiforme (EM)
- A spectrum that includes EM minor at one end and EM major (SJS/TENS) at the other end
- Busulfan, cyclophosphamide, diethylstilbestrol (DES), hydroxyurea, MTX, mitomycin C, mitotane.
Erythema multiform minor
- Characterized by the target like lesion distributed on the palms and soles, no mucosal involvement.
Erythema multiform major
- Steven Johnson syndrome is sometimes termed as erythema multiform major. There is mucosal involvement.
Severe Cutaneous Adverse Reactions
- Type 4 hypersensitivity reaction
- SCARS involve the skin and mucous membranes of various body openings. May also involves serious damage to internal organs.
- Most common culprit drugs are Allopurinol, Anticonvulsants, NSAIDs,
- Sulfa drugs, Bumetanide, Captopril, Furosemide, Penicillamine, Piroxicam, Thiazide diuretics, Antipsychotic, Trimethoprim-Sulfamethoxazole.
It includes a group of five diseases:
- Drug reaction with eosinophilia and systemic symptoms (DRESS Syndrome)
- Steven Johnson Syndrome
- Toxic Epidermal Necrolysis
- SJS/TEN Overlap Syndrome
- Acute generalized exanthematous pustulosis (AGEP)
a. DRESS Syndrome
Drug reaction with eosinophilia and systemic symptoms
Characterized by fever, skin rash, lymphadenopathy, hematological abnormalities, and internal organ involvement (liver, kidney).
Potentially life-threatening
Delayed hypersensitivity reaction to drugs; Antiepileptics, Antipsychotics, Allopurinol. Latency period 2- 6 weeks
b. Steven Johnson syndrome and Toxic Epidermal Necrosis
Sloughing of skin and mucosa
Target lesions and mucosal involvement most commonly involved mucosa are oral cavity and conjunctiva. Extensive involvement of respiratory mucosa can lead to respiratory failure and the need for mechanical ventilation.
These two diseases may be considered as a spectrum of severity of the same disease with TEN being a more severe form
The difference is a function of involved total body surface area as follows:
- < 10% BSA involved: SJS
- 10-30% BSA involved: SJS/TEN overlap
- > 30% BSA involved: TEN

Sore throat, red conjunctiva, oral ulceration and target lesion, Positive nikolsky sign
Drugs commonly involved are Penicillins, Sulfa drugs, NSAIDS, Phenytoin, Phenobarbital.
c. AGEP
Pustular drug eruption/Toxic pustulosis
Characterized by the eruption of sterile pustules 2-5 days after exposure to a drug commonly distributed in the flexure regions; armpit, groin.
Associated with fever, malaise, multiorgan involvement, although rare but fatal
Persists for one to two weeks and then the skin peels off with desquamation as it resolves.
Clinical notes
By going through this you will get to know which aspects of the eruption you have to focus to develop diagnosis and managing pt.
How to deal with a case of drug eruption
a. Relevant Points in History
Sudden Symmetric cutaneous eruptions in any pt. taking any medication.
- The temporal relation of eruption with drug
- Evolution and progression of the lesion
- Any previous history of an allergic reaction to any drug
- Any known allergic illness ( allergic rhinitis, atopic eczema, asthma)
- Family history of atopic disorders
- Any concurrent disease or comorbidity
- Note down all medication pt. is using at the time of presentation
- Any association of eruption with any particular stuff.
- History of photosensitivity.
Take proper detailed history and do examine
- the lesions so to rule out any other etiology
b. Relevant Dermatological Examination
- Monitoring Vital signs is very important in SJS/TEN Patient (Blood pressure, Temperature, Respiratory rate, Pulse)
- Lymphadenopathy (SCARS, serum sickness)
- Inspect whole skin & its appendages
a. Inspect mucosal membranes for any lesion or swelling
Describe the lesion/s as a function of:
- Distribution & Symmetry (acral, extensor, flexural, truncal, nonspecific)
- Total body surface area (BSA) involved in disease
- Size & Number
- Morphology
- Bullous eruption (Bulla tense/flaccid, nikolsky sign)
- Configuration (discrete/confluent)
- Shape (discoid, annular, target)
- Borders (well/poorly defined)
- Color (hypo/hyperpigmented, erythema)
- Are all the lesions of the same type and age
- If not of the same age note the pattern of evolution (for that you should know the fate of lesion).
c. Relevant Investigations
- Complete blood count (CBC) with differential count
- Serum chemistry studies (liver and renal function test)
- Biopsy of the lesion
- Antibody or immunoserology tests
- Direct cultures from wound/ ruptured bullous lesion
- Patch testing
The suspected drug patch is applied to the skin for 48 hours development of papules, vesicles or edema will show a type IV reaction to that drug.
- In Vitro tests: Examples include basophil degranulation test, lymphocyte transformation test.
- Intradermal test: The suspected drug is injected intradermal wheal formation shows a type I reaction to that drug
d. Treatment
Discontinue the offending drug
Supportive care:
- Pain medication
- Hydration
- Sterile wound care
Systemic immune modulators:
- Steroid
- Antihistamine
- Intravenous immunoglobulins
- Immunosuppressive agents
Hospital admission in burn ICU settings for SJS/TENS
Treat any concurrent infection
e. Prevention
Educate patient about drug eruption and offending drug which has to be avoided in future.
She is a compassionate individual with excellent presentation, research, and communication skills. Organized and driven with an impressive list of achievements and excelling within high-pressure environments, she is skilled at applying various learning methods and tools to make study easy. She is interested in reading and writing medicine-related articles.