Case Scenario
A 3 year boy form Western region presented at Emergency Room in a state of altered sensorium. The child was well 5 days back, but since then he is been having fever and loose stool. The episode of illness started with fever, measured upto 102 F, was on and off type and relieved by Paracetamol. The child had loose stool 3-4 episode per day, was small amount, greenish-yellow with blood and mucus.
On the 3rd day of fever and loose stool, the child passed reddish urine and the urine output decreased progressively and significantly compared to before. And on next day the child had altered sensorium, the child used to shout and was restless and was disoriented. Parents noticed pallor in the child and child looked fairer than before.
However, there was no history of loss of consciousness or seizure but there was a doubtful history of tonic posturing. The child did not have cough or cold. The child was able to breastfeed. There was no history of:
- Rashes over the body, petechie/purpura
- Joint pain or swelling
- Abdominal pain or vomiting
- Burning micturation, straining during urination or foul smelling urine
- Recurrent UTI in the past
On examination
The child appeared pale; there was no icterus or edema. There were no signs of dehydration.
- BP – 120/70 mmHG (high for his age)
- RR – 28/min, regular
- PR – 110/min, regular and good volume
- Temp – 99 F
- JVP was not raised
- Saturation was maintained without O2
The child was well nourished. There were no rashed over the body. ENT examination was normal.
Chest: B/L equal air entry, Normal vesicular Breath sounds, no added sounds.
CVS: Heart sounds were normal, no murmurs heard
Per abdomen: soft, non tender, no organomegaly, Normal bowel sound
CNS:
- Glasgow Coma Scale – 11/15
- Pupils – B/L reacting to light, equal size.
- No focal cranial deficits.
- Motor and sensory system were intact.
- No Cerebellar or Meningeal signs
Genital/Musculoskeletal systems: normal findings
Making a Clinical Diagnosis
With the History, we first thought of Acute Glomerulonephritis – probably PSGN which is the commonest cause. Hematuria, Hypertension and Oliguria were in favour of this diagnosis. Encephalopathy was explained by hypertension. But the age of onset was against it.
Dysentry with Acute Renal failure was another diagnosis and we thought altered sensorium was due to Uremic encephalopathy. But the thing that was not matching was the episode of loose stool which wasn’t significant enough to cause Acute renal failure and the child did not look dehydrated.
Hemolytic Uremic Syndrome seemed to strongly match with this case. With the history of diarrhea and typical onset of symptoms on 3rd day of diarrhea. Pallor and renal impairment were both explained by it. Encephalopathy was due to Uremia or hypertension secondary to Renal impairment. Age also was in favour of it. So Typical / Diarrhea+ve Hemolytic Uremic Syndrome was thought of. One thing that striked us was, the Fever and altered sensorium with suspected seizure.
Thrombotic thrombocytopenic purpura could be another possibility but the onset was too rapid and age was against it as TTP occurs mainly in older age.
We could not over-rule Sepsis with organ dysfunction as it was one of the likely cause in background of fever, thrombocytopenia and AKI and we considered it in our workup plan.
Investigations
CBC – Hb-7.9 g%; WBC- 44,000 with 54 N 43 L; Nucleated RBC – 54/100 WBC (corrected WBC would have been normal for the age); Platelets – 43,000
Urea – 180mg/dl, Creatinine – 3.3mg/dl, Na – 145, K – 4.8
Calcium – 8.8, Phosphate – 8.8
RBS-120mg/dl
LFT – normal
Chest Xray – normal
Urine RME – Normal
Management
Inj. Ceftriaxone was started.
Inj. Lasix challenged was tried (though we had in mind that it wasn’t helpful in intrinsic renal failure)
As Blood Pressure was not controlled and there was no urine output, Tab. Nifedipine was started.
Intravenous fluid was started with 400ml/BSA for the 1st day.
Preparation for Hemodialysis was made. HIV/HBsAg/Anti HCV serology were non reactive. PT/INR was normal. Repeat sample of urine showed Albumin +++ and ASO titre was Normal.
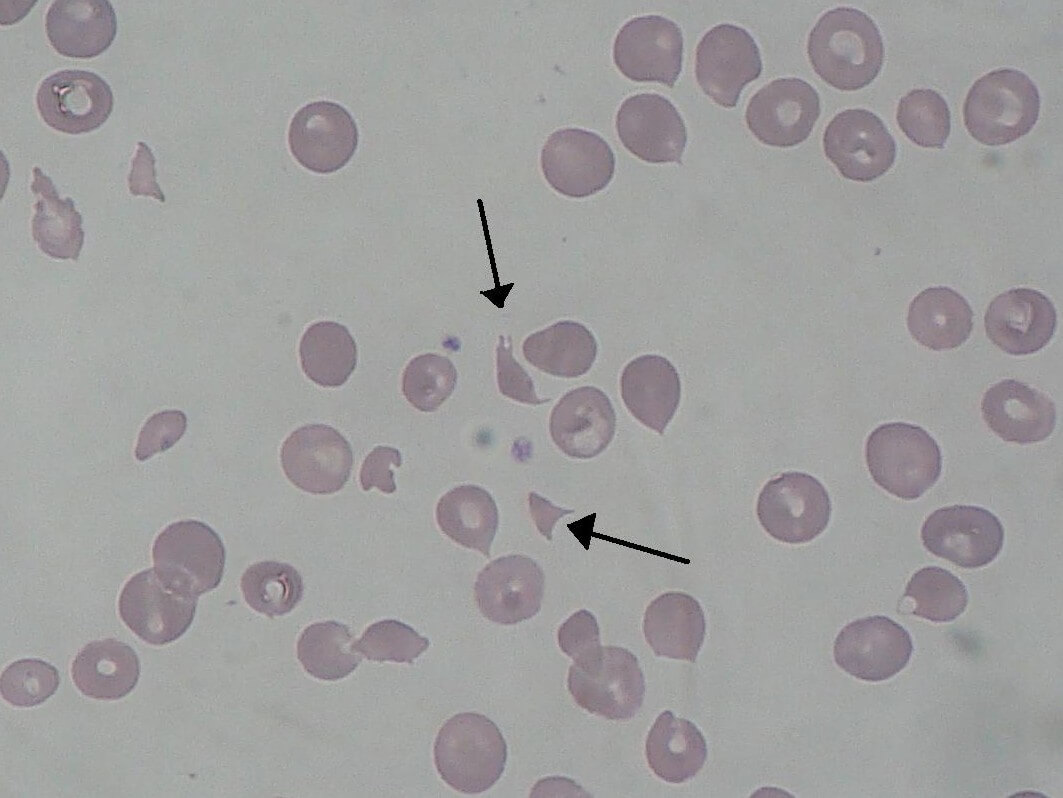
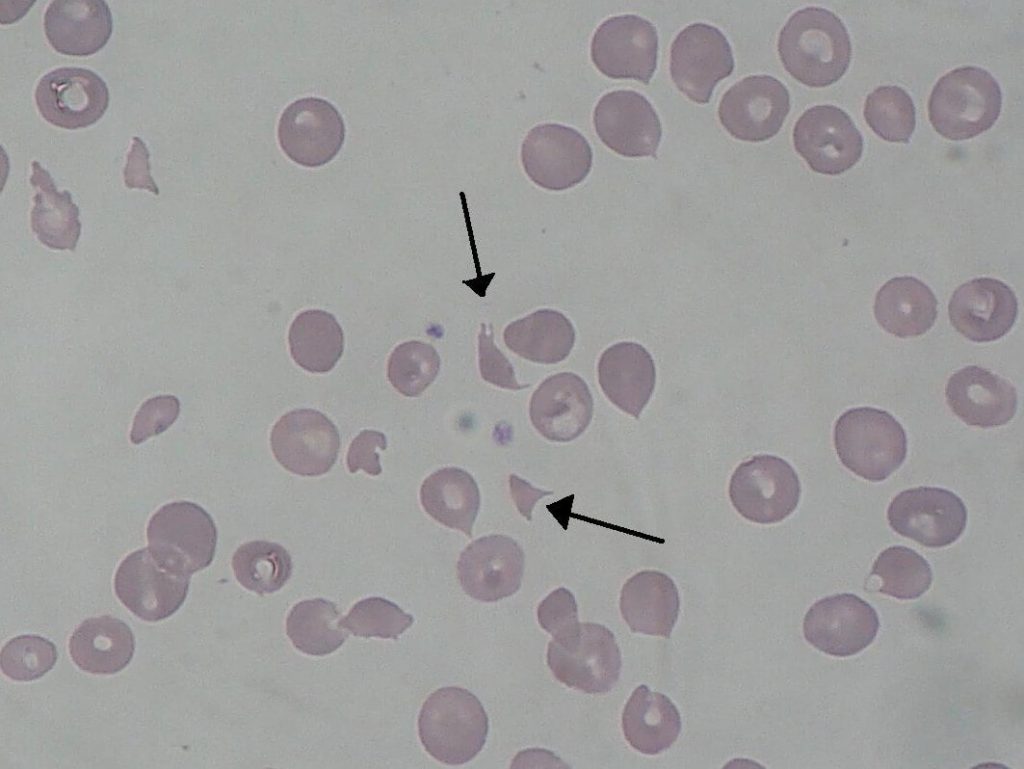
Peripheral Smear reports showed – fragmented RBCs, polychromasia and Normocytic normochromic RBCs with Retics – 1.8%.
Now we had, HUS as our diagnosis, still TTP could be a possibility. We consulted Nephrology unit to discuss on the possible need of Plasmapheresis which wa thes 2nd line treatment for HUS and 1st line for TTP.
Hemodialysis was done for 1 hour with drastic improvement in sensorium and wellness of the child. So we deferred plasmapheresis at the moment. Urine improved from nil to 0.2ml/kg/hr. Blood transfusion was carried out during HD.
Conclusion
This was one Classic case of Hemolytic Uremic Syndrome. Any child of smaller age group with history of diarrhea/dysentery and progressive pallor and renal impraiment, HUS should be one of the differentials.
If you have any suggestions or you want to add your differential diagnosis, comment section is open for you.

MD Pediatrics and Fellowship Neonatology, he chooses to stay anonymous. He often writes his views online as well as share few important topics for medical students, doctors and specially parents. He does research in pediatrics.