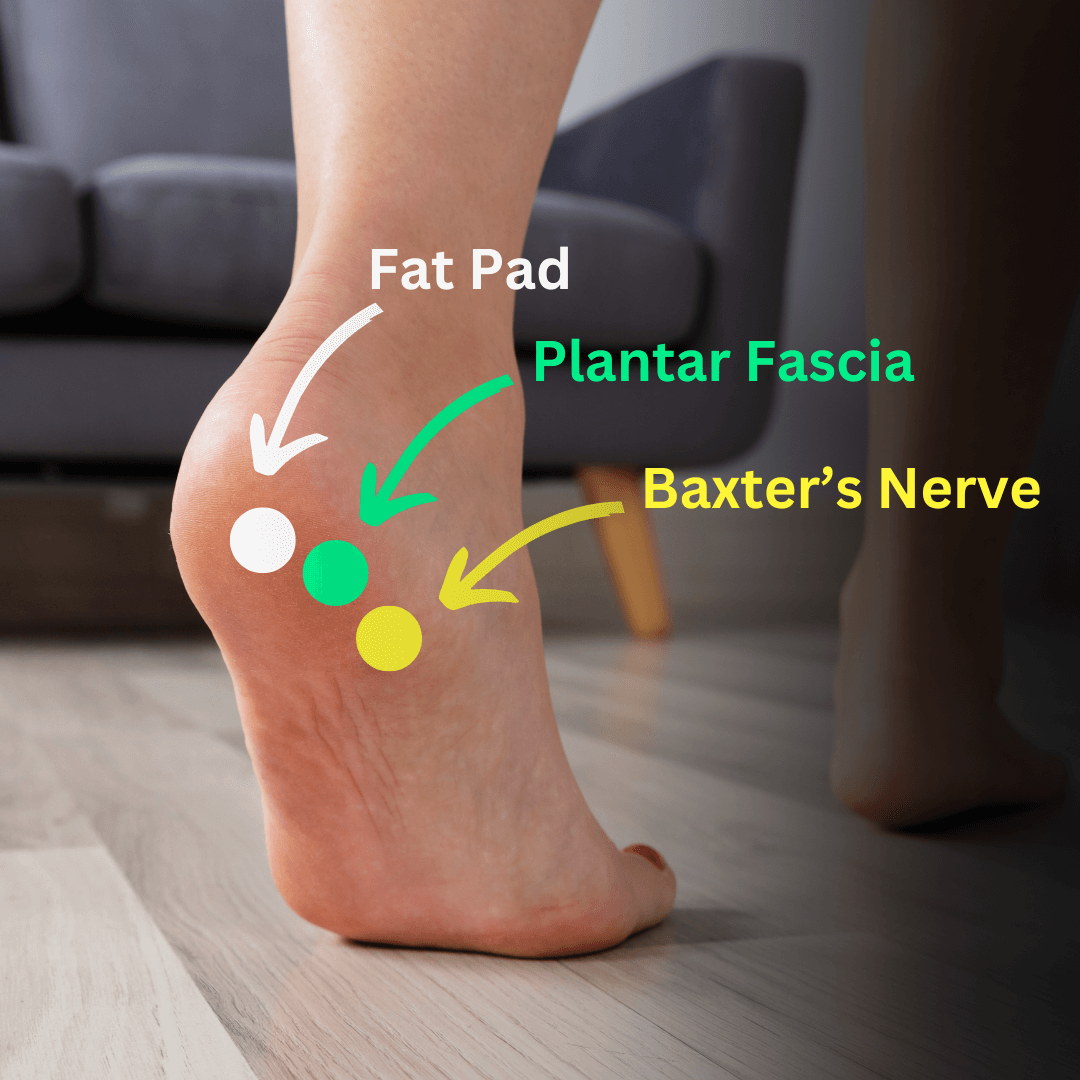
Heel pad syndrome and plantar fasciitis both cause heel pain, but they affect different areas and have distinct characteristics.
Further reading and differential diagnoses of heel pain: Heel Pain : Mnemonic
| Plantar Fasciitis | Heel Pad Syndrome | |
| Definition | Inflammation of the calcaneal origin of plantar fascia | Traumatic irritation of the specialized fat that covers & protects calcaneus |
| Pain | Medial calcaneal border pain with first steps, aggravated by walking or standing | Central calcaneal pain aggravated by walking or standing |
| Tenderness | Localized tenderness at calcaneal origin of plantar fascia – in the midline or slightly medial of midline at the origin of the longitudinal arch of the foot. | Entire bottom of heel is tender (if tenderness if present at calcaneal origin of plantar fascia it is not more painful than the rest of the heel) |
| Calcaneal compression | Painful (mild) | Painless |
| Heel pad compression | Painless | Painful |
| Achilles tendon flexibility | May be limited in cases with duration of 2-3 months | Normal |
| Treatment – Initial | 1. Heel cups 2. Padded arch supports 3. Avoid tiptoeing or pressure across the ball of feet & limit standing/walking 4. Ice application to heel 5. Achilles tendon stretching exercises 6. Massage over heel with rubber ball | Treatment same as for plantar fasciitis from 1-4. Not much role of physiotherapy |
| Treatment – Persistent cases (3-4 weeks) | 1. NSAIDs 2. Taping of ankle & arch to support arch 3. Re-emphasize use of padding | 1. Limit weight bearing & continue heel cups |
| Treatment – Persistent cases (6-8 weeks) | 1. Obtain foot X-rays 2. Local steroid injection + Immobilization using high-top shoes with soft arch support 3. Repeat injection in 4-6 weeks if symptoms have not improved by 50% + Air cast or short leg walking cast 4. Custom made arch supports (for pes planus or pes cavus) | No injection |
| Treatment – Chronic cases (3-4 months) | Possible surgical intervention | No surgical procedure |
Heel pad syndrome: Patients with an uncomplicated heel pad syndrome should have resolution of symptoms and signs within 2-3 weeks when treated with proper padding of the heel. Patients with persistent symptoms should be evaluated for stress fracture of calcaneus, plantar fasciitis, or subtalar joint inflammation.
Plantar fasciitis: Corticosteroid injection combined with padded arch supports and limited weightbearing is successful in approximately 60% of cases. Persistent or recurrent fasciitis (approximately 10% of cases) is seen most often in patients with obesity, with abnormal arch and ankle conditions, with calcaneal spurs greater than 1/2 to 3/4 inch in length, or with jobs demanding prolonged standing or walking on concrete surfaces.
Reference: Office Orthopedics for Primary Care – Treatment, 3rd Edition (Bruce Carl Anderson)