EPIDEMIOLOGY OF BREAST CANCER
Incidence: In general, less industrialized nations tend to have lower rates of breast cancer, with Japan being an exception to this rule. The highest rates are seen in Europe and North America.
Age at onset:
- Estrogen receptor (ER)-positive cancer: incidence rates increase rapidly until approximately age 50 (proportional to the seventh power of the age), and then rise slowly (proportional to the first power of the age). ER-positive tumors are more likely to occur in postmenopausal women.
- ER-negative cancer: incidence increases rapidly before age 50 (proportional to the fifth power of the age) and then remains constant.
Race: incidence is higher among white women than African- American woman, but the mortality is higher for the latter owing to late presentation and socio-economic factors. Breast cancers in African Americans are more likely to be early-onset, higher-grade, and ER-negative compared with those in whites.
RISK FACTORS FOR BREAST CANCER
1. Increased duration of exposure to endogenous estrogen:
- Early menarche (<12 yrs): reduction in risk of 5% to 10% for each year delay in age at menarche
- Late menopause (>55 yrs): increase in risk of 3% for each year delay in age of menopause
- Late age at 1st pregnancy: after 35 years of age had 40% to 60% higher risk than those who had a first child before 20 years of age
- Risk initially increases after the 1st pregnancy due to significant elevated hormonal levels and rapid proliferation of breast, then decreases after 10 years owing to epithelial cell differentiation leading to decreased sensitivity to carcinogens (longer cell cycles and more time for DNA repair)
- Breastfeeding: relative risk of breast cancer decreased by 4.3% for every 12 months of breastfeeding
- Delayed re-establishment of ovulation
- Differentiation of epithelial cells
- Obesity (high BMI): 1.25 to 2 times increased risk in postmenopausal women
- premenopausal: protective due to lower estradiol levels
- postmenopausal: increased risk of breast cancer due to higher estradiol level resulting from conversion of androgens by aromatase enzyme in adipose tissue
2. Exogenous hormones (Oral Contraceptive Pills):
- 24% greater risk compared with never-users
- risk disappeared after discontinuing
- no relation with duration of use pre-menopausal
- in postmenopausal women, risk increased by 2.3% for each year of use and the relative risk was 1.35 for women who had used hormones for 5 or more years.
- estrogen only (relative risk 1.3) and estrogen + progestin (relative risk 1.5 to 2.0)
3. Lifestyle and dietary factors:
- Alcohol consumption: relative risk increases of 32% for consumption of 35 to 44 g/day and 46% for 45 g/day or more
- Physical activity: protective effect with risk reduction ranging from 10 to 50%
- Soy and phytoestrogens: protective owing to competition of phytoestrogens (known generally as isoflavones) with endogenous estrogen for binding to estrogen receptors, as well as other possible anticarcinogenic effects
4. Ionizing radiation (Environmental factor):
- risk is higher in women exposed before age 20 years and is small for exposure after age 40 years
- before age 40, there is a positive correlation between radiation dose and breast cancer risk
- 8X increased risk was documented in women with Hodgkin disease who received radiotherapy dose of more than 40 Gy
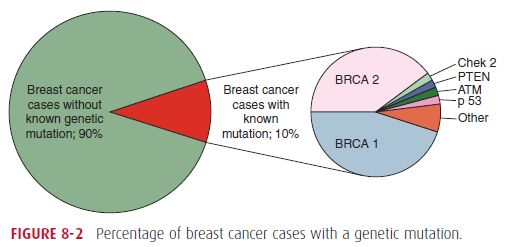
5. Genetic factors:
- Family history:
- If mother or sisters had breast cancer: ~ 2X increased risk
- Factors further increasing the risk: multiple affected family members, early onset of disease, bilateral breast cancer, and affected male
- High penetrance genes:
- BRCA1 gene (17q21) and BRCA2 (13q12-13)
- Deleterious mutation in the 2 genes ~ 10X relative risk
- Li-Fraumeni syndrome (germline mutation in p53): increased risk of leukemia and cancers of brain, breast and lungs
- Cowden syndrome (PTEN mutation)
- Low penetrance genes:
- CHEK2, ATM, BRIP1, PALB2, NBS1, and RAD50.
- Mutations associated with 2-4X increased risk
6. Benign breast disease:
- Nonproliferative breast disease (eg. fibroadenoma, cysts, adenosis): relative risk 1
- Proliferative breast disease without atypia (eg. adenosis, intraductal papilloma): relative risk 1.5-2
- Atypical hyperplasia: relative risk 5 (atypical lobular hyperplasia > ductal hyperplasia)
- DCIS/LCIS: relative risk 8-10
7. Mammographic density:
- Connective and epithelial tissue has a high radiologic density, whereas fat appears translucent
- Women with the most extensive mammographic density (as a percentage of total area imaged) have a 2- to 6-fold greater risk, compared to those with low to absent density
| Mnemonic | Factors | Description | Protective |
|---|---|---|---|
| A | Age | >50 years | Mammography 3 yearly from 50-70 years (from 40 years if high risk) |
| B | Benign breast conditions | Proliferative without atypia (1.5-2X) Atypical hyperplasia (5X) | |
| C | Cancer | Cancer of contralateral Breast (3-4X) Cervix, Ovary, Colon, Prostate Radiation Therapy for Hodgkin’s Lymphoma | |
| D | Diet | Alcohol Phytoestrogen Deficiency | Vitamin C |
| E | Estrogen | Nulliparous Obese Postmenopausal Women Exogenous Estrogen (OCP, HRT) | Breast feeding Late Menarche Early Menopause Early age at 1st childbirth |
| F | Familial History | 2-10X risk in family history of Breast, Colon, Ovarian and Prostate carcinoma | |
| G | Genetics | BRCA 1 BRCA2 (Male breast cancer) p53 PTEN (Cowden) | |
| G | Geography | African American | Rare in Japan and Taiwan |


A GOOD INFORMATION TO KNOW YOUR MODIFIABLE AND MNON MODIFIABLE RISK FACTORS.