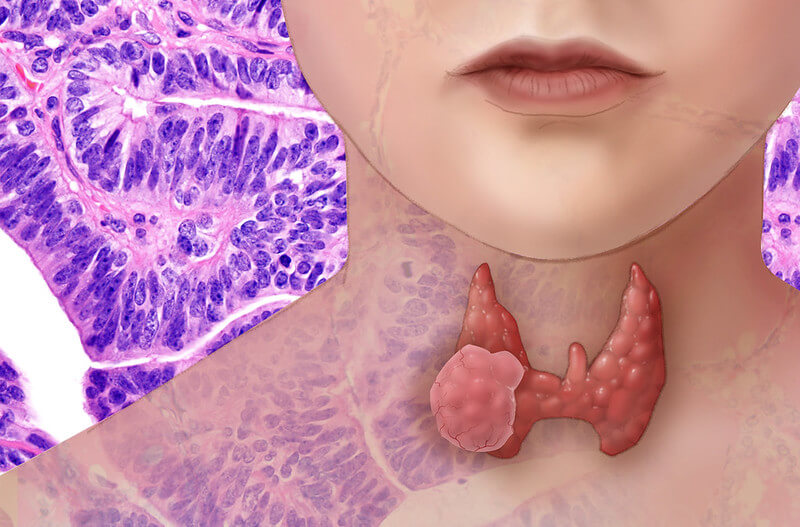
When Maria noticed her necklace felt tighter and colleagues asked if she’d gained weight, she didn’t think much of it. But within weeks, swallowing her morning coffee became uncomfortable, and her voice turned raspy. A visit to her doctor revealed goiter—an enlarged thyroid gland pressing against her windpipe and vocal cords. Maria’s experience is shared by millions worldwide, yet many don’t recognize the early warning signs or understand what’s happening inside their neck.
Goiter isn’t a single disease. It’s a visible symptom of underlying thyroid dysfunction, ranging from harmless swelling to conditions that demand urgent intervention. This guide walks you through what goiter really is, why it develops, how doctors diagnose it, and what treatments—from iodine pills to surgery—can restore your health and peace of mind.
What Is Goiter and Why It Matters
Goiter means an abnormal enlargement of the thyroid gland, the butterfly-shaped organ at the base of your neck. The thyroid produces hormones that regulate metabolism, energy, heart rate, and body temperature. When the gland swells—whether from nutrient deficiency, autoimmune attack, or nodule growth—it can disrupt hormone balance and compress nearby structures like the trachea and esophagus.
Crucially, most goiters are benign. They’re not cancer. But any persistent neck lump warrants evaluation because a small percentage harbor thyroid cancer or precancerous cells. Early assessment ensures you receive the right care, whether that’s watchful waiting, medication, or surgery.
Understanding the difference between goiter and thyroid hormone imbalance is key. You can have an enlarged gland with normal hormone levels (euthyroid goiter), too much hormone (hyperthyroidism), or too little (hypothyroidism). Each scenario requires a tailored approach, which is why accurate diagnosis matters so much.
Symptoms of Goiter and When to Seek Care
Early goiters may cause no symptoms at all. You might notice a subtle fullness in your neck or feel your shirt collar tighten. As the gland grows, symptoms become more obvious:
- Visible neck swelling or a palpable lump at the base of the throat
- Hoarseness or voice changes when the gland presses on the recurrent laryngeal nerve
- Difficulty swallowing (dysphagia) or a sensation of food sticking
- Breathing difficulty or cough, especially when lying flat, if the goiter compresses the trachea
- Fatigue, weight changes, mood swings when hormone levels shift up or down
Seek immediate medical attention if you experience:
- Rapidly enlarging neck mass over days or weeks
- Stridor (high-pitched breathing sound) or severe shortness of breath
- New-onset severe hoarseness or complete voice loss
- A hard, fixed nodule that doesn’t move when you swallow
- Pain, fever, or redness suggesting infection or bleeding
These red flags may signal retrosternal extension (goiter extending into the chest), acute thyroiditis, or, rarely, aggressive thyroid cancer. Prompt evaluation can prevent life-threatening airway compromise.
Causes and Risk Factors for Goiter
Goiter develops when the thyroid enlarges in response to a trigger. The most common causes worldwide include:
1. Iodine Deficiency
Iodine is essential for thyroid hormone synthesis. When dietary iodine is low, the thyroid grows larger to capture more iodine from the bloodstream. This endemic goiter remains the leading cause globally, especially in regions without iodized salt programs. Foods rich in iodine – seaweed, dairy, fish, iodized salt can prevent or reverse deficiency-related goiter if caught early.
2. Autoimmune Causes: Graves’ Disease and Hashimoto’s Thyroiditis
Graves’ disease triggers the immune system to produce antibodies (TRAb) that overstimulate the thyroid, causing hyperthyroidism and diffuse goiter. Hashimoto’s thyroiditis, the most common autoimmune thyroid disorder, generates antibodies (anti-TPO) that attack thyroid tissue, leading to chronic inflammation, gland enlargement, and eventual hypothyroidism. Both conditions create sustained thyroid hormone imbalance and often present with goiter as an early sign.
Thyroiditis – acute, subacute, or postpartum can also cause transient gland swelling, tenderness, and fluctuating hormone levels before resolving or progressing to chronic disease.
3. Other Causes and Risk Factors
- Multinodular goiter: Multiple benign nodules grow within the gland, sometimes producing excess hormone (toxic multinodular goiter) or causing mechanical compression
- Solitary thyroid nodules: A single lump that may be benign (colloid nodule, adenoma) or malignant
- Medications: Lithium, amiodarone, and certain antithyroid drugs can enlarge the thyroid
- Pregnancy: Rising hCG and increased iodine demand can temporarily enlarge the gland
- Family history: Genetic predisposition to autoimmune or nodular thyroid disease
- Radiation exposure: Childhood head/neck radiation increases nodule and cancer risk
- Smoking: Thiocyanate in tobacco smoke acts as a goitrogen
- Age and sex: Women over 40 face higher risk of thyroid disorders
Types of Goiter You Might Hear About
Doctors classify goiters by structure, function, and location to guide treatment decisions:
1. Diffuse vs. Nodular vs. Multinodular Goiter
Diffuse goiter involves smooth, uniform enlargement of the entire gland, typical in Graves’ disease or iodine deficiency. Multinodular goiter features multiple discrete lumps of varying size. These nodules can be autonomous (producing hormone independently), creating thyroid hormone imbalance and symptoms of hyperthyroidism, or they may grow large enough to compress the esophagus and trachea, causing dysphagia and dyspnea.
2. Toxic vs. Nontoxic; Retrosternal Goiter
Toxic nodular goiter means one or more nodules overproduce thyroid hormone, leading to hyperthyroidism – weight loss, palpitations, heat intolerance, and anxiety. Nontoxic goiter maintains normal hormone levels but may still cause compressive symptoms.
Substernal or retrosternal goiter extends below the collarbone into the chest cavity. Because it occupies limited space near the airway and great vessels, even modest growth can trigger breathing difficulty, especially when lying down or raising the arms. Retrosternal goiters often require surgical removal due to compression risk.
Diagnosis and Evaluation: What to Expect
Accurate diagnosis begins with a thorough history and physical exam, followed by blood tests and imaging to map the gland and assess cancer risk.
History, Physical Exam, and Thyroid Function Tests
Your doctor will ask about symptoms, medication use, dietary iodine, family history, and radiation exposure. Palpation reveals gland size, texture, nodules, and tenderness. Blood tests measure:
- TSH (thyroid-stimulating hormone): Low TSH suggests hyperthyroidism; high TSH indicates hypothyroidism
- Free T4 and T3: Direct hormone levels to confirm thyroid function
- Thyroid antibodies: Anti-TPO and TRAb identify autoimmune disease (Hashimoto’s, Graves’)
Imaging and Additional Tests
Thyroid ultrasound is the first-line imaging tool. It maps nodule size, echotexture, calcifications, and vascularity – features that help stratify cancer risk. Radionuclide uptake scan (I-123 or Tc-99m) shows whether nodules are “hot” (hyperfunctioning, usually benign) or “cold” (non-functioning, higher malignancy risk).
When goiter extends into the chest or compresses the airway, CT or MRI provides detailed anatomical assessment to plan surgery safely.
Fine-Needle Aspiration (FNA) and Cancer Risk
Ultrasound-guided FNA biopsy samples suspicious nodules to detect or rule out thyroid cancer. Indications include nodules 1 cm or larger with worrisome ultrasound features (irregular margins, microcalcifications, taller-than-wide shape, increased vascularity). Risk stratification systems such as the Bethesda classification guide whether to observe, repeat FNA, or proceed to surgery based on cytology results.
Treatment Options for Goiter: From Monitoring to Surgery
Treatment depends on goiter size, symptoms, hormone status, and cancer risk. Options range from watchful waiting to radioactive iodine therapy and thyroidectomy.
Watchful Waiting and Medical Management
Small, asymptomatic goiters with normal thyroid function may simply be monitored with periodic exams and ultrasound. Iodine supplementation effectively treats and prevents iodine-deficiency goiter, though excess iodine can worsen autoimmune thyroid disease. Levothyroxine (synthetic T4) is prescribed for hypothyroid goiter (e.g., Hashimoto’s) to normalize TSH and potentially reduce gland size, though results vary.
Shrinking a goiter with medication alone works best when the cause is reversible iodine deficiency or early hypothyroidism but has limits. Multinodular goiters and large compressive goiters rarely shrink significantly with pills alone.
Treating Overactive (Toxic) Goiters
Antithyroid drugs—methimazole (preferred) or propylthiouracil (PTU)—block thyroid hormone synthesis, controlling hyperthyroidism in Graves’ disease or toxic nodular goiter. Treatment typically lasts 12–18 months, with regular blood monitoring for liver function and white blood cell counts. Relapse is common after stopping medication.
Radioactive iodine (RAI) therapy uses I-131 to selectively destroy overactive thyroid tissue. Candidates include patients with toxic nodular goiter, Graves’ disease, or large goiters who prefer a permanent solution. After a single oral dose, the radioactive iodine concentrates in the thyroid and shrinks the gland over 3–6 months. Most patients develop hypothyroidism post-RAI and require lifelong levothyroxine, but symptoms of hyperthyroidism resolve.
Surgery for Goiter (Thyroidectomy)
Thyroidectomy is recommended when:
- The goiter compresses the airway or esophagus, causing breathing or swallowing difficulty
- FNA reveals suspicious or malignant cells
- Large multinodular goiter distorts neck anatomy or extends retrosternally
- Medical therapy fails to control hyperthyroidism, or the patient prefers definitive treatment
Procedure types: Total thyroidectomy removes the entire gland; lobectomy (hemithyroidectomy) removes one lobe. The choice depends on nodule location, cancer risk, and whether both lobes are affected.
Risks include recurrent laryngeal nerve injury (causing hoarseness or voice change in 1–2% of cases), hypocalcemia from parathyroid gland damage (temporary in 10–30%, permanent in 1–3%), bleeding, and infection. Experienced endocrine surgeons minimize these risks through careful technique and intraoperative nerve monitoring.
Recovery: Most patients go home the same day or next morning. Calcium and vitamin D supplements may be needed if parathyroid function is impaired. Thyroid hormone replacement (levothyroxine) begins immediately after total thyroidectomy, with doses adjusted based on TSH levels. Follow-up includes neck ultrasound and lab tests to monitor for recurrence or hormone imbalance.
Lifestyle, Diet, and Natural Remedies (Complementary)
While lifestyle changes alone rarely cure goiter, they support thyroid health and may slow progression or improve symptoms when combined with medical treatment.
Nutrients That Support Thyroid Health
Iodine: Essential but not risk-free. Adequate intake (150 mcg/day for adults) from iodized salt, dairy, fish, and seaweed prevents deficiency-related goiter. Excess iodine, however, can trigger or worsen autoimmune thyroid disease. Supplements should only be taken under medical guidance.
Selenium and zinc: Both minerals support thyroid hormone metabolism and immune function. Food sources include Brazil nuts (selenium), shellfish, meat, seeds, and whole grains. Supplementation may help patients with Hashimoto’s thyroiditis reduce antibody levels and inflammation, but evidence is mixed and doses should be modest.
What to Limit and Lifestyle Tips
Goitrogens are compounds in certain foods that can interfere with iodine uptake or thyroid hormone synthesis. Raw cruciferous vegetables (broccoli, kale, cabbage), soy products, and millet contain goitrogens. Cooking generally inactivates them, and unless you consume massive amounts or have iodine deficiency, they pose little risk to most people.
Smoking cessation is critical. Thiocyanate in tobacco smoke acts as a goitrogen and worsens thyroid disease. Medication review is important—discuss lithium, amiodarone, and other drugs that affect the thyroid with your doctor. Avoid unverified supplements marketed to “detox” or “boost” the thyroid; many contain excessive iodine or interfere with prescribed medications.
Possible Complications and Outlook
Potential Complications
Untreated or large goiters can lead to:
- Compressive symptoms: Dysphagia, dyspnea, and stridor from tracheal or esophageal obstruction
- Hyperthyroidism effects: Atrial fibrillation, osteoporosis, heart failure if toxic nodules go unchecked
- Hypothyroidism effects: Weight gain, depression, high cholesterol, and cardiovascular disease from untreated hormone deficiency
Long-Term Outlook and Monitoring
With appropriate treatment, most patients enjoy excellent outcomes. Small goiters may stabilize or shrink with iodine or hormone therapy. Surgery and RAI offer definitive solutions for larger or toxic goiters. Regular follow-up—physical exams, ultrasound, and thyroid function tests—detects recurrence early. Managing underlying causes (autoimmune disease, iodine status) reduces the risk of new nodules or gland re-enlargement.
Evaluation and Treatment at Liv Hospital
Liv Hospital in Istanbul offers comprehensive, patient-centered care for goiter, combining advanced diagnostics with expert medical and surgical treatment.
Why Choose Liv Hospital for Goiter Care
The multidisciplinary team—endocrinologists, head and neck surgeons, radiologists, and pathologists—collaborates to design personalized treatment plans. Services include state-of-the-art ultrasound imaging, ultrasound-guided fine-needle aspiration, modern thyroidectomy techniques with nerve monitoring, and radioactive iodine therapy in a single, coordinated location.
Liv Hospital’s endocrine surgery unit is staffed by surgeons experienced in complex and retrosternal goiter cases, minimizing complications and optimizing recovery. The endocrinology department manages pre- and post-operative hormone levels, ensuring seamless transitions from diagnosis through long-term follow-up.
What to Expect and How to Get Started
The journey begins with a thorough diagnostic evaluation: history, physical exam, thyroid function tests, ultrasound, and FNA if indicated. Based on results, observation, medication, RAI, or surgery is discussed, tailored to symptoms, lifestyle, and preferences. Post-treatment care includes close monitoring, hormone replacement guidance, and rehabilitation support to restore quality of life.
International patient assistance is available. Liv Hospital welcomes patients from around the world and provides support with airport transfers, accommodation, translation, appointment scheduling, and follow-up consultations via telemedicine.
Quick FAQs About Goiter
Can goiter be cancer? When is biopsy needed?
Most goiters are benign. Biopsy (FNA) is recommended for nodules 1 cm or larger with suspicious ultrasound features or rapid growth to rule out malignancy.
How to shrink a goiter naturally and when it’s not enough?
Adequate iodine, selenium, and avoiding goitrogens may help small goiters. Large, symptomatic, or toxic goiters require medication, RAI, or surgery for effective control.
Will thyroidectomy affect my voice? What are the risks?
Experienced surgeons use nerve monitoring to protect the recurrent laryngeal nerve. Voice changes occur in 1–2% of cases; most are temporary.
Is multinodular goiter dangerous? Does it cause hormone imbalance?
Multinodular goiter can produce excess hormone (toxic) or compress nearby structures. Regular monitoring and timely treatment prevent complications.
Can I have a healthy pregnancy with goiter?
Yes, but thyroid function must be optimized before and during pregnancy. Work closely with an endocrinologist to adjust medication and monitor TSH.
How long does radioactive iodine therapy take to work?
RAI shrinks the goiter and controls hyperthyroidism over 3–6 months. Symptom improvement begins within weeks, with full effect by six months.
If you’re experiencing neck swelling, difficulty swallowing, or unexplained fatigue, early evaluation can identify the cause, rule out serious disease, and restore thyroid health with expert care.