Collagen accounts for nearly 30% of all body proteins and is the major structural part of the extracellular matrix in connective tissues. Collagen fibrils, which confer tensile strength and elasticity to skin, tendons, ligaments, cartilage, and bone, consist mainly of glycine, proline, and hydroxyproline. Its endogenous production gradually decreases after the third decade of life, with an estimated annual decline of 1–1.5%, reinforced by ultraviolet radiation, glycation, and oxidative stress. This is one reason for many of the dermatological and rheumatological signs related to aging. Oral administration of hydrolyzed collagen peptides-usually 2.5-15 g daily-has therefore been explored in RCTs to assess its potential to counteract such deficiency. The sections below review the mechanistic pathways and clinical evidence related to skin, hair, nails, joints, and ancillary systems, with a focus on bioavailability and therapeutic dosing.
Biochemical and Pharmacokinetic Considerations
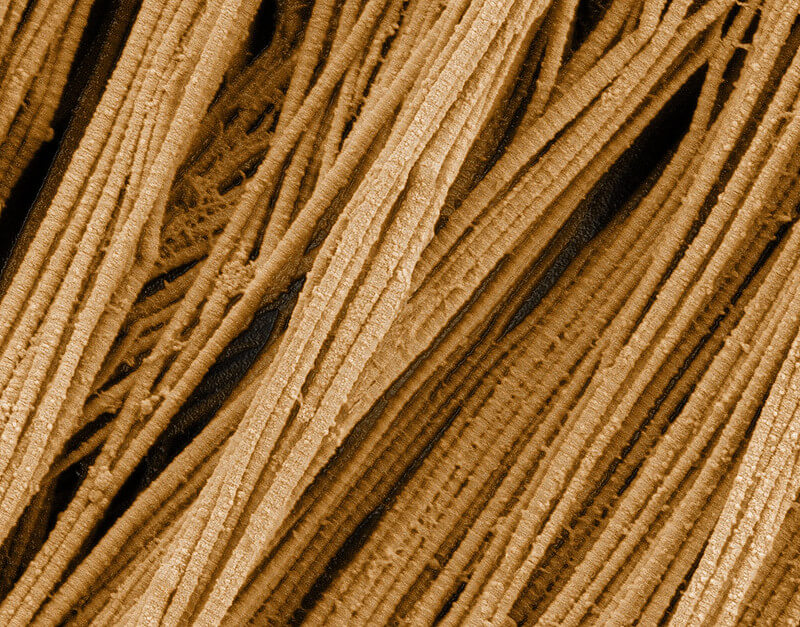
Hydrolyzed collagen of molecular weight 2-6 kDa has >90% bioavailability, while peak plasma concentrations of proline-hydroxyproline dipeptides are reached within 1-2 hours. These bioactive peptides stimulate fibroblast proliferation through integrin-mediated signaling and upregulate transforming growth factor-β, enhancing de novo collagen synthesis. Type I and III collagens predominate in the dermis and hair follicles, whereas type II is cartilage-specific; multi-source formulations may therefore confer broader efficacy.
Dermatological Outcomes
A double-blind RCT involving 69 women aged 35-55 years demonstrated that 2.5 g daily of bioactive collagen peptides increased skin elasticity by 7% (p<0.05) and reduced the volume of periorbital wrinkles by 20% after 8 weeks, measured via cutometry and PRIMOS optical 3D analysis. Hydration improved concurrently, which was attributable to enhanced hyaluronic acid synthesis. Meta-analysis of 11 studies (n=805) confirms a standardized mean difference of 0.54 (95% CI 0.35-0.72) favoring collagen for skin elasticity.
Trichological and Onychological Effects
Nail fragility and hair tensile strength reflect keratinocyte matrix integrity. In a prospective cohort of 25 with brittle nail syndrome, 2.5 g collagen daily for 24 weeks reduced nail peeling by 42% and increased growth rate by 12%. Trichological benefits include reduced telogen effluvium; however, evidence remains preliminary and warrants larger RCTs.
Articular and Cartilage Integrity
Type II collagen peptides, 40 mg/day undenatured or 10 g/day hydrolyzed, improve symptoms in osteoarthritis. A 2016 multicenter RCT (n = 190) described a 38% reduction in WOMAC pain scores and 33% improvement in Lequesne index after 13 weeks of treatment with 10 g hydrolyzed collagen, with MRI evidence of cartilage preservation. Mechanisms include downregulation of matrix metalloproteinase-13 and interleukin-1β.
Additional Systemic Benefits
- Gastrointestinal: Collagen peptides reinforce the tight junctions and thereby may attenuate increased intestinal permeability.
- Osteology: Co-supplementation with calcium and vitamin D increases bone mineral density in postmenopausal women by 1.23% in the lumbar spine compared to placebo.
- Musculotendinous: 15 g collagen plus vitamin C before exercise increases patellar tendon cross-sectional area in athletes.
Clinical Implementation
Daily doses of 5-15 g, dissolved in aqueous media, are normally well-tolerated with very minimal adverse effects. Amino acid profile fidelity is greater when hydrolyzed peptides from grass-fed bovine or marine-derived sources are used. Type II collagen-enriched formulations are indicated for targeted joint therapy. Physicians could refer patients to certain resources for evidence-based options on collagen powder supplement, ensuring that they align with the patient’s individual clinical profile. In conclusion, supplementation of collagen peptides represents a safe and bioavailable intervention with moderate-to-large effect sizes across integumentary and musculoskeletal domains. Integration into preventive and therapeutic protocols is supported by the accumulation of Level I evidence.