Terminologies Related with Status Epilepticus
1. Seizure: Abnormal or excessive neuronal discharge causing a transient disturbance of cerebral function.
2. Epilepsy: A condition characterized by recurrent (≥2) unprovoked seizures.
3. Status Epilepticus (SE):
a. Conventional definition: 2 fits occur without recovery of consciousness in between or a single fit lasts longer than 30 minutes with or without loss of consciousness.
The rationale behind the time limit of 30 minutes is that – irreversible neuronal injury may occur after 30 minutes of seizure activity.
b. New ILAE task force definition:
- A condition resulting either from:
- Failure of the mechanisms responsible for seizure termination or
- From the initiation of mechanisms
- Leading to abnormally prolonged seizures (after time point t1) i.e. demarcation of time when treatment should be initiated
- Tonic-clonic SE: 5 min
- Focal SE with impaired consciousness: 10 min
- Absence SE: 10-15 min
- And can have long-term consequences (after time point t2) – including neuronal death, neuronal injury, and alteration of neuronal networks, depending on the type and duration of seizures.
- Tonic-clonic SE: 30 min
- Focal SE with impaired consciousness: 60 min
- Absence SE: Unknown
4. Refractory Status Epilepticus: SE not responding to atleast:
- 2 doses of Benzodiazepines, followed by
- Phenytoin/valproate and
- Phenobarbitone or midazolam infusion beyond 60 minutes after the treatment has started.
Classification of Status Epilepticus
A) With Prominent Motor Symptoms:
- Convulsive SE (Tonic-clonic)
- Myoclonic SE (Prominent epileptic myoclonic jerks)
- Focal motor: Repeated focal motor seizures (Jacksonian), Epilepsia Partialis Continua (EPC), Adversive status, Oculoclonic, Ictal paresis
- Tonic SE
- Hyperkinetic SE
B)Without Prominent Motor Symptoms (Non-convulsive i.e. NCSE):
- NCSE with coma
- NCSE without coma
- Generalized: Typical absence, Atypical absence, Myoclonic absence
- Focal: Without impairment of consciousness, Aphasic status, With impaired consciousness
- Autonomic SE
Etiology of Status Epilepticus
1. Known (Symptomatic):
Acute:
- Sudden antiepileptic withdrawl
- Stroke
- Intoxication
- Metabolic disorders (hypoglycemia, hyponatremia)
- Alcohol or Benzodiazepine withdrawl
- Malaria
- Encephalitis
Remote: Post-traumatic, Post-encephalitic, Post-stroke, etc.
Progressive: Brain tumor, Lafora’s disease and other Progressive Myoclonic Epilepsy (PME), Dementia
SE in defined Electroclinical syndromes
2. Unknown (Cryptogenic)
Differentiating Status Epilepticus from Pseudostatus
Management of Convulsive Status Epilepticus
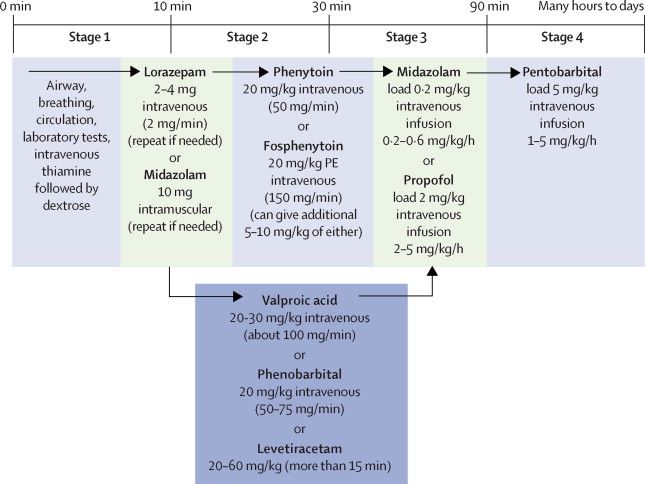
The management of Status Epilepticus has been updated as per new algorithm by American Epilepsy Society (2016) with few modifications:
0-5 minutes: Stabilization phase
1. Airway, Breathing, Circulation, Disability examination as in trauma protocol.
2. Connect the monitors, assess vital signs, give oxygen (nasal cannula or face mask) and initiate ECG monitorning.
3. Consider intubation if respiratory assistance required.
4. Rule out hypoglycemia with finger stick blood glucose test: If glucose <60 mg/dl –
- Adults: 100 mg thiamine IV then 50 ml D50W IV
- Children ≥2 years: 2 ml/kg D25W IV
- Children <2 years: 4 ml/kg D12.5W IV
Why thiamine needs to be given before dextrose?
If the patient happens to be thiamine deficient, the PDH (Pyruvate Dehydrogenase) reaction for converting Pyruvate to Acetyl-CoA requiring TPP (Thiamine pyrophosphate) cofactor doesn’t work leading to shunting of pyruvate to lactate formation. Without thiamine replacement, all glucose supplemented would go into pathway of lactate formation – exacerbating the lactic acidosis.
Thiamine supplementation is relatively inexpensive and harmless.
5. Attempt IV access – collect blood sample for electrolytes, hematology, toxicology screen, anticonvulsant levels (if appropriate).
5-20 minutes (Initial therapy phase)
Benzodiazepines: Any one of the following –
During status epilepticus, the number of active GABA receptors progressively decrease with time and they become less effective.
Benzodiazepines at higher concentrations also inhibit sustained repetitive neuronal firing, as with carbamazepine and phenytoin.
1. IM midazolam stat:
- 13-40 kg: 5 mg
- >40 kg: 10 mg
2. IV lorazepam (may repeat dose once):
- 0.1 mg/kg/dose, max 4 mg/dose at the rate 2 mg/min
Currently, lorazepam is preferred over diazepam because:
- Duration of action is longer (less chances of recurrent seizures) – it’s antiepileptic effects starts after 5 minutes and lasts for 12 hours compared to diazepam whose antiepileptic effect starts after 3 minutes and wanes off after 30 minutes.
- Fewer adverse reactions including cardiorespiratory depression.
3. IV diazepam (may repeat dose once):
- 0.15-0.2 mg/kg/dose, max 10 mg/dose at the rate 5 mg/min
In community settings and when IV access is not possible:
1. Rectal diazepam single dose (not repeated) can be considered –
- Children >12 years and Adults: 10-20 mg (0.2 mg/kg)
- Children <12 years: 0.5 mg/kg
2. Buccal midazolam:
- Adults: 10-20 mg
- Children: 0.4-0.5 mg/kg
3. Intranasal midazolam:
- Adults: 5 mg
- Children: 0.2 mg/kg
Equivalent dose of Benzodiazepines:
Chlordiazepoxide 25 mg = Temazepam 10 mg = Diazepam 5 mg = Lorazepam 1 mg = Alprazolam 0.5 mg = Clonazepam and Triazolam 0.25 mg
Move to next phase only if seizure is uncontrolled.
20-40 minutes (Second therapy Phase)
Any one of the following –
1. IV Phenytoin or Fosphenytoin (Under ECG and BP monitoring):
Phenytoin: Bolus of 1 gm (adults) or 20 mg/kg IV at 25-50 mg/min (1 mg/kg/min) OR
- Maximum: 1 gm/dose
Fosphenytoin 20 mg PE (1.5 mg Phosphenytoin = 1 mg Phenytoin)/kg at 100-150 mg PE/minute – total dose <1500 mg PE/dose
- Maximum: 1.5 gm Phenytoin equivalent/dose
Fosphenytoin (aqueous parenteral ester prodrug of phenytoin) avoids the local tissue reactions associated with phenytoin, but otherwise probably has the same ADR as phenytoin, including cardiovascular ADRs (cardiac arrhythmias, QT prolongation, hypotension).
Phenytoin possess risk of local reaction due to high alkalinity. To avoid, following measures are recommended –
- It shouldn’t be given through the same line as other medications.
- It shouldn’t be given with glucose soultions.
- It should be followed by flushing with sterile saline.
- Continuous infusion should be avoided.
Fosphenytoin can be used with intramuscular route (IM) if necessary.
2. IV valproic acid (single dose):
- 40 mg/kg (max 3 gm/dose)
3. IV levetiracetam (single dose):
- 60 mg/kg (max 4.5 gm/dose)
If none of the options are available: IV phenobarbital (single dose) 15 mg/kg at <100 mg/min (maximum dose for adults: 1 gm).
40-60 minutes (Third therapy phase)
Repeat Second therapy phase or use Anesthetic doses of either: Thiopental, Midazolam, Pentobarbital or Propofol
Neonatal seizures
The guidelines are opted from Newbornwhocc.
1. 1st line drug: IV phenobarbitone 20 mg/kg over 20 minutes (<1 mg/kg/min)
- Additional dose of 10 mg/kg may be repeated every 20-30 minutes until a total dose of 40 mg/kg.
2. 2nd line drug:
WHO recommended: Midazolam or Lidocaine
Appropriate for NICU settings in Nepal and India: IV Phenytoin 20 mg/kg at <1 mg/kg/min (diluted in equal volume of NS; are incompatible with dextrose solutions).
- Repeate dose of 10 mg/kg may be tried for refractory seizures.
3. 3rd line drugs:
Lorazepam: 0.05 mg/kg IV bolus over 2-5 minutes; may be repeated OR
Midazolam: 0.15 mg/kg IV bolus followed by infusion of 0.1 to 0.4 mg/kg/hour
Diazepam is not recommended due to narrow therapeutic index.
4. If refractory to above treatment: Lidocaine, Paraldehyde, Sodium valproate, Vigabatrin or Topiramate
5. Last resort: IM pyridoxine 50 mg (1 ml) in each gluteal region/anterolateral thigh (total 100 mg) in NICU setting (hypotension and apnea can occur).
References:
1. Glauser T, Shinnar S, Gloss D, et al. Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Currents. 2016;16(1):48-61. doi:10.5698/1535-7597-16.1.48.
2. A Clinical Guide to Epileptic Syndromes and their Treatment By C. P. Panayiotopoulos
3. Manno EM. Status Epilepticus: Current Treatment Strategies. The Neurohospitalist. 2011;1(1):23-31. doi:10.1177/1941875210383176.