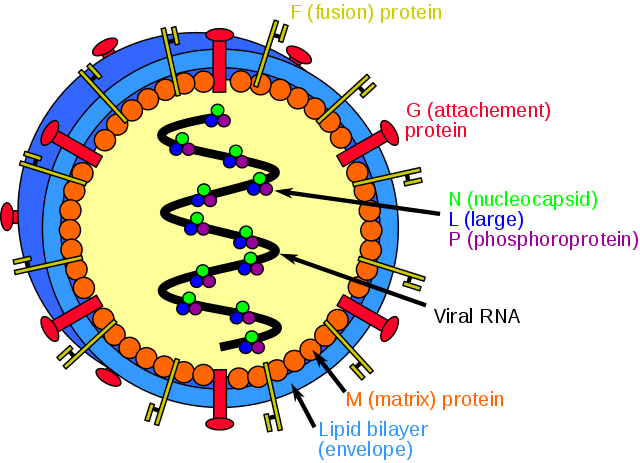
Nipah virus is closely related to, but distinct from Hendra virus.
Family: Paramyxoviridae
Genus: Henipavirus
History:
- A Nipah epidemic of viral encephalitis, complicated by respiratory failure, occurred in Malaysia in 1998 and 1999, causing 265 infections and 105 fatalities (93% had occupational exposure to pigs).
- An associated outbreak among abbatoir (slaughter-house) workers in Singapore during March 1999 led to 11 cases of infection and 1 fatality. The causative agent, isolated from cerebrospinal fluid, was later named Nipah after the town that was most affected.
- Nipah virus was later also identified in India and Bangladesh in 2001, with the flying fox (Pteropus spp.) as the natural host, although no intermediate animal host was found in more recent outbreaks there.
Distribution:
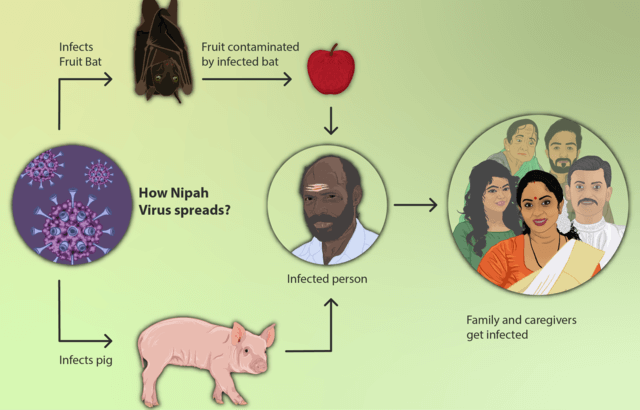
- Natural hosts: Fruit bats (distributed accross an area that encompasses the northern, eastern, and southeastern sections of Australia, Indonesia, Malaysia, Philippines, and some of the Pacific islands).
- Apparent source of infection: Infected pigs
- Evidence of infection in cats and dogs has also been found.
- There is evidence that nosocomial transmission of Nipah is possible.
Presentation:
- Incubation period: 4-18 days
- Animals are infectious during incubation period. It is unknown whether humans are infectious during incubation, but this should be considered probable.
- Clinical symptoms range from mild to fatal.
- 3-14 days of fever, sore throat, headaches, muscle pain, and respiratory symptoms.
- Onset is usually flu like.
- This may be followed by drowsiness, dizziness, disorientation, and rapid progression into coma.
- The patient may develop flaccid paralysis and may require ventilatory support.
- Hypotension and bradycardia may precede death.
- Case fatality rate approaches 50%.
Diagnosis:
- CSF can show Nipah virus by vero-cell culture with a subsequent electron microscopy.
- Immunofluorescence and IgM ELISA have also been used to detect viruses in tissues of CNS, lungs, and kidneys of both infected humans and swine.
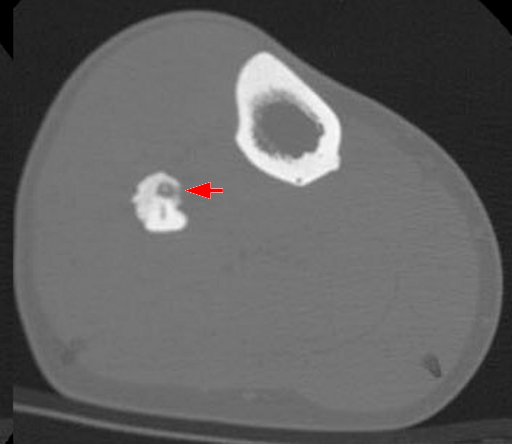
- MRI changes in brain are distinct from other paramyxoviridae encephalitis.
Treatment:
- No drug therapies.
- Intensive supportive therapy is the sole treatment.
- Early treatment with antiviral ribavirin may reduce the duration and severity of infections.