- Change in consistency of stool: Increased water-content
- Increase in freqency of stool: >3 times per day
- Increase in weight of stool: >200 grams per day or >10 grams/kg/day
Among all these, diarrhea is best explained by the change is consistency of the stool. Acute diarrhea is short-lived i.e. less than 2 weeks.
CAUSES OF ACUTE DIARRHEA
1. Infectious:
- Viral (more common): Rotavirus, Norwalk (calcivirus), Adenovirus, Astrovirus
- Bacterial:
- With or without dysentery: Enterohemorrhagic E.coli, Shigella, Campylobacter, Plesiomonas shigelloides, Salmonella
- Without dysentery: Enterotoxigenic E.coli, Enteropathogenic E.coli, Vibrio cholera, Aeromonas, Bacillus cereus, Clostridium difficile, Clostridium perfringes, Staphylococcus aureus
- Parasitic:
- With or without dysentery: Entamoeba histolytica, Trichuris trichuria
- Without dysentery: Giardia lamblia, Cryptosporidium parvum, Cyclospora cayetanensis, Isospora belli
- Fungal: Candida albicans
2. Non-infectious:
- Drugs: Antibiotics and laxatives
- Allergic colitis
- Lactose intolerance
- Radiation/Chemotherapy enteritis
- Appendicitis
- Niacin deficiency (Pellagra)
- Copper or Zinc toxicitiy
EPIDEMIOLOGICAL TYPES OF ACUTE DIARRHEA
1. Community acquired diarrhea
2. Hospital acquired diarrhea:
- Onset of diarrhea 3 days after hospitalization and not incubating at the time of admission to hospital
- Related to antibiotic use , non-antibiotic medications or tube feeds
PATHOGENESIS OF ACUTE DIARRHEA
In healthy adults, 93% of fluid entering the intestines is absorbed by the time it reaches the ileocecal valve. Children become volume depleted more rapidly than adults (due to an increased surface/volume ratio and limited renal compensatory capacity). Loss of electrolytes in stool:
- Sodium: 20-25 mEq/L
- Potassium: 50-70 mEq/L
- Chloride: 20-25 mEq/L.
| Osmotic diarrhea | Secretory diarrhea | |
| Response to fasting | Diarrhea stops | Diarrhea continues |
| Volume of stool | <200 ml/day | >200 ml/day |
| Stool Na+ | <70 mEq/l | >70 mEq/l (Increased Na+ and K+ secretion in stool) |
| Stool osmotic-gap i.e. 2 (Na + K) | >100 mOsm/kg | <50 mOsm/kg |
| Reducing substances | Positive | Negative |
| Stool pH | <5 |
|
- Osmotic diarrhea: Lactose intolerance, Malabsorption via damaged intestinal epithelial cells (rotavirus, shigella, etc.)
- Secretory diarrhea: Via enterotoxins or invasion of bowel mucosa
ASSESSMENT OF DEGREE OF DEHYDRATION
| Symptom/Signs | Mild (A) | Moderate (B) | Severe (C) |
| Look: | |||
| General condition | Alert, active | Restless, irritable | Lethargic, unresponsive |
| Eyes | Normal | Slightly sunken | Very sunken |
| Tears | Normal | Decreased | Absent |
| Thrist | Normal | Eagerly drinking | Not able to drink |
| Feel: | |||
| Skin pinch | Instant recoil | Recoil in <2 sec | Recoil in >2 sec |
| Other things to be looked (not in IMCI guidelines) | |||
| Respiratory rate | Normal | Normal; fast | Deep |
| Heart rate | Normal | Normal or increased | Increased or decreased when most severe |
| Pulse volume | Normal | Normal or decreased | Weak/impalpable |
| CRT | Normal | Prolonged | Prolonged, minimal |
| Anterior fontanelle | Normal | Depressed | Depressed |
| Extremities | Warm | Cool | Cool, mottled, cyanotic |
| Urine output | Normal to decreased | Decreased | Minimal |
HISTORY FOR ACUTE DIARRHEA
- Diarrhea – Onset, duration, frequency, pattern, severity
- Dysentery – Blood/mucus?
- Osmotic vs secretory – fasting reduces stooling amount (osmotic)?
- Small bowel vs large bowel diarrhea?
- Associations –
- Gastrointestinal: nausea, vomiting, anorexia, abdominal pain
- Respiratory tract infection: fever, cough, coryza
- Arthralgia/arthritis and rash
- Recent family history or contact history
- Underlying disease, recent infections, medications, HIV
- Incubation period: shorter in toxigenic than inflammatory diarrhea
- Temporal relation with food
| Small bowel diarrhea | Large bowel diarrhea | |
| Stool | Large volume, watery | Frequent, small volume |
| Associated features | Abdominal cramps, bloating, gas | Gripping pain in lower abdomen |
| Fever | Not common | Common |
| Tenesmus | Absent | Present |
| Blood or mucus in stool | Absent | Present |
PHYSICAL EXAMINATION FOR ACUTE DIARRHEA
- Assess for severity of dehydration
- Abdominal tenderness/mass? Peritoneal signs?
- Perianal inspection: Rash? Ulcer? Active bleeding?
- Stool if present: Blood? Mucus?
- Extraintestinal signs: Rash? Hepatosplenomegaly? Lymphadenopathy? Arthritis?
- Hypokalemia: Abdominal distension? Muscle strength and reflexes?
INVESTIGATIONS FOR ACUTE DIARRHEA
1. Serum electrolytes (Volume depletion)
2. BUN and serum creatinine:
- Significant rise in BUN with relatively normal creatinine suggests dehydration
- If RFT is markedly deranged: screen for HUS, including coagulation studies and markers of hemolysis (LDH, Peripheral blood smear, Haptoglobin)
3. CBC with differential count:
- Infection: Abnormal WBC or differential count
- Dehydration: Increased hematocrit
- HUS: Anemia and thrombocytopenia
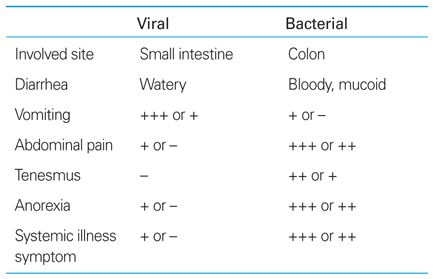
Risk factors for bacterial etiology:
- Age <6 months
- Immunocompromised
- Weight <8 kg
- Severe (>5 episodes/24 hour)
- History of prematurity
- Bloody diarrhea
- Fevere
- Moderate to severe dehydration
- Failed ORS therapy
- Nonbloody to bloody diarrhea within 5 days of onset
- Abdominal pain and tenderness
- Pain worse with defecation (especially E.Coli O157:H7)
- Rectal prolapse (Shigellosis and E.Coli O157:H7)
- Minimal vomiting
- Recent antibiotic use
Vomiting and respiratory symptoms are common in viral etiology of acute diarrhea.
Lab investigations for supsected bacterial etiology:
- Stool culture including E.Coli O157:H7, C.difficile assay, Giardia, Cryptosporidia assay
- Fecal WBC
- Consider:
- Fecal occult blood
- Blood culture
- Urine culture
- Abdominal X-ray
CONSIDER HOSPITAL ADMISSION
- Inability to care or return if necessary
- Intractable vomiting
- Inadequate ORS intake because of refussal
- Lack of improvement
- Co-morbid illness
- Severe dehydration
- Other risk factors
TREAT DEHYDRATION (IMCI guidelines)
Plan A: No signs of dehydration (Mild dehydration)
- Treat at home
- ORS per each loose stool:
- <24 months (with Tea spoon): 50-100 ml
- 2-10 years (Cup sips): 100-200 ml
- >10 years (Cup sips): Ad lib
- Teach ORS preparation
- If vomiting: wait 10 minutes and feed slowly
- If ORS packet used up, give other fluids
Plan B: Some signs of dehydration (Moderate dehydration)
- Treat at home or hospital
- Provide daily requirement
- Replace deficit:
- ORS 75 ml/kg over 4 hours OR by NG tube
- Assess after 4 hours:
- If still “some signs of dehydration”: Continue deficit replacement
- If improved to “no signs of dehydration”: ORS 10 ml/kg per stool
Plan C: Severe dehydration
- Treat at hospital
- Intravenous Ringer Lactate:
- For <12 months:
- 1st hour: 30 ml/kg (repeat if feeble pulse)
- Next 5 hours: 70 ml/kg
- For >12 months:
- 1st 1/2 hour: 30 ml/kg
- Next 2 and 1/2 hours: 70 ml/kg
- OR NG feeding 20 ml/kg/hr until IV opened
- For <12 months:
- Reassess every 15-30 minutes
- Shift plan of treatment according to improvement or continue same treatment
Dehydration at tertiary centers can be treated as following:
1. Stabilization: Bolus 20 ml/kg upto 3 times
2. Deficit replacement: According to the severity of dehydration
3. Maintenance fluid: (Daily requirement* – Bolus amount) over 24 hours
- Half of total in 1st 8 hours
- Other half in next 16 hours
Daily requirement* = 4 ml/kg/hr for 1st 10 kg + 2 ml/kg/hr for next 10 kg body weight + 1 ml/kg/hr for subsequent body weight
Causes of ORS failure:
- High purge rate >5 ml/kg/hr
- Persistent vomiting >3/hr
- Paralytic ileus
- Incorrect ORS preparation
Content of ORS:
- Glucose 13.5 gm/L
- Na+ 2.6 gm/L
- K+ 1.5 gm/L
- Citrate 2.9 gm/L
Total osmolarity: 245 mmol/L
MEDICAL THERAPY FOR ACUTE DIARRHEA
1. Antibiotics: Antibiotic therapy is usually not indicated because illnesses are often self-limited. Indications for antibiotic therapy are:
- Shigella, Enterotoxigenic E.Coli, Enteroinvasive E.Coli, Salmonella typhi, Vibrio cholera
- Extraintestinal infections (including sepsis) and complications
- Infants (<3 months)
Antibiotics for uncomplicated Salmonella is contraindicated as it may prolong the “carrier-state”.
Antibiotics used are:
- C.difficile: Metronidazole 7.5 mg/kg Or Vancomycin 10 mg/kg
- Shigella: Azithromycin 10 mg/kg/day Or Ceftriaxone 50 mg/kg/day X 3 days
- Salmonella: Ceftriazone 100 mg/kg/day BD Or Azithromycin 20 mg/kg/day X 7 days
- E.Coli O157:H7: None
- Enteroinvasive E.Coli: As shigella
- V.Cholera: Erythromycin 30 mg/kg/day divided TID OR Azithromycin 10 mg/kg/day X 3 Days
- Giardiasis: Metronidazole 15 mg/kg TDS X 5-7 days OR Tinidazole 50 mg/kg PO once (max 2 gm) OR Nitazoxanide
- Cryptosporidium: Nitazoxanide
- ETEC, EAEC, Traveller’s diarrhea: Azithromycin or Ceftriaxone X 3 days
2. Antidiarrheals: not recommended because it may cause abdominal distension and bacterial overgrowth
3. Zinc supplementation: 20 mg Elemental Zinc/day for child >6 months X 14 days
4. Ondansetron: 0.1-0.2 mg/kg/dose
5. Potassium (if patient is passing urine): KCl 30-40 mEq/L
6. Antisecretory (inhibit intestinal enkephalinase): Racecadotril
7. Probiotics: contains Lactobacillus rhamnosus, Enterococcus fecium, Saccharomyces boulardii
8. Vaccine: Rotavirus
NUTRITIONAL MANAGEMENT FOR ACUTE DIARRHEA
- Avoid simple sugar foods (Carbonated beaverages, commercial fruit juices, sweetened tea)
- Early feeding reduces infection induced permeability
- BRAT (Banana, Rice, Apple sauce, Toast) are overly restrictive and increases recovery time
- Age appropriate unrestricted diet must be given – complex carbohydrates, meats, yoghurt, fruits, vegetables
7 Basic principles of Management of Acute Diarrhea:
- Give ORS when possible
- ORS must be started within 3-4 hours
- Age appropriate unrestricted diet must be given after dehydration correction
- Continue breastfeeding
- Diluted formula is not recommended
- Replace ongoing losses with ORS
- Minimize unnecessary lab investigation/medication