Date of writing: June 17, 2025
Day 3 of my pre-fellowship was unlike the others – not because I scrubbed in for an arthroplasty or a hip case (there weren’t any today), but because I witnessed firsthand how a routine trauma case can spiral into an anatomical and surgical challenge.
Case: A left distal humerus fracture, AO Type C2. The complexity of anatomic fixation of fracture was expected. What wasn’t expected, however, was an iatrogenic transection of ulnar nerve around the cubital tunnel during exposure and handling.
There was a moment of collective pause in the Operation Room – the kind of silence that says, “This just got serious.”
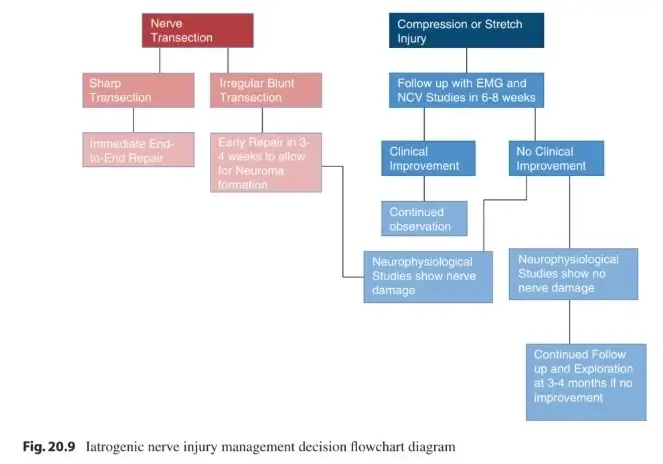
The nerve was immediately explored, ends freshly debrided, and an epineural repair was performed using 6-0 prolene. What I realized today is that trauma surgery is not just about bone alignment. It’s about safeguarding everything around it.
Literature review
The incidence of ulnar neuropathy after surgery for distal humerus fractures varies between 0% and 51%, with an average of 12%.
a. Immediate Direct Repair is Ideal:
For sharp transections of mixed nerves, such as the ulnar nerve, immediate tension-free epineural repair offers the best chance for regeneration. This allows:
- A single junction for regenerating axons to cross
- Preserved vascularity on both nerve ends
- Avoidance of neuroma or glioma formation due to delayed fibrosis
- Better motor recovery than delayed repair or grafting
b. Outcomes of Immediate Repair vs Grafting:
- 73% recovery rate with immediate repair
- 56% with nerve grafting
The sharp nature of the injury and immediate repair in your case favors the better outcome group.
c. Time Sensitivity:
Delay beyond days leads to stump retraction, swelling, and fibrosis, making direct repair without tension increasingly difficult.
d. Prognosis Considerations for Elbow-Level Injuries:
- Ulnar nerve injuries at the elbow denervate both intrinsic hand muscles and forearm flexors (FDP, FCU).
- Due to the long distance to intrinsic hand muscles, motor recovery is typically poor even after repair – because of 1% loss of motor end plates per week.
Despite this, early repair is still essential to preserve extrinsic motor function and protective sensation.
e. Sensory vs Motor Recovery:
- Sensory recovery has better potential (68% meaningful recovery even in proximal injuries)
- Motor recovery – especially intrinsic hand muscle function remains limited (often <60%), though early repair improves odds.
Further reading: Management of Iatrogenic Ulnar Nerve Transection – PMC

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music. He is currently pursuing Fellowship in Hip, Pelvi-acetabulum and Arthroplasty at B&B Hospital.