Skin – Systemic Disease Connection
“When a man has on the skin of his body a swelling or an eruption… and the disease appears to be deeper than the skin it is a leprous disease.” – Leviticus 13: 2-3
In ancient times changes in skin were taken to indicate the whole body was diseased and there was clearly an appreciation of the connection between skin and systemic illness.
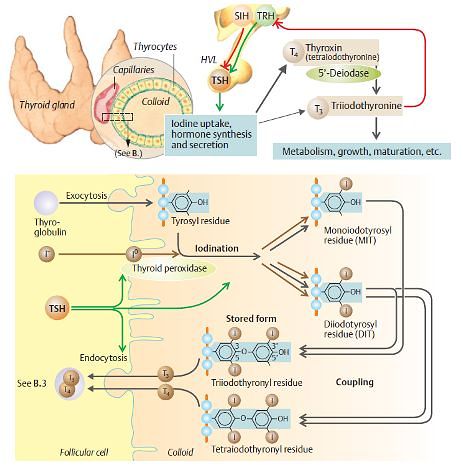
Thyroid gland and hormones
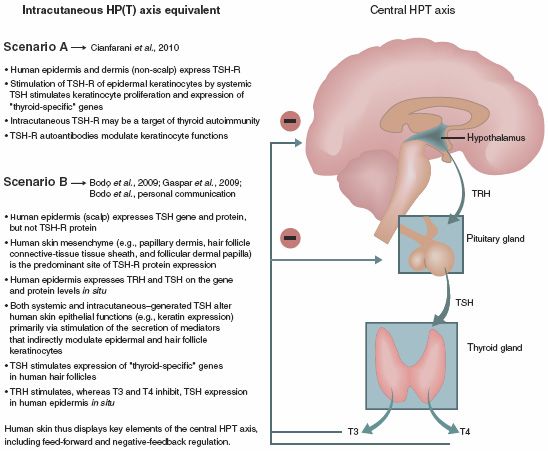
Thyroid – Skin Connection
- Direct thyroid hormone action on skin is mediated through Thyroid Hormone Receptor (TR).
- Tri-iodothyronine (T3) has been shown to stimulate growth of both epidermal keratinocytes and dermal fibroblasts.
- Thyroxine (T4) stimulates the proliferation of hair follicle keratinocytes and T3 inhibits their apoptosis.
HYPERTHYROIDISM
Causes:
- Grave’s disease
- Toxic multinodular goiter
- Toxic adenoma
- Subacute thyroiditis
- Postpartum thyroiditis
- Silent thyroiditis
- Excessive iodine ingestion
- Exogenous thyroid ingestion or Overmedication
General skin changes
A) Warm
- Increased cutaneous blood flow
B) Moist
- Reflection of underlying metabolic state
C) Smooth
- Epidermis is thin but not atrophic, and the stratum corneum is well hydrated
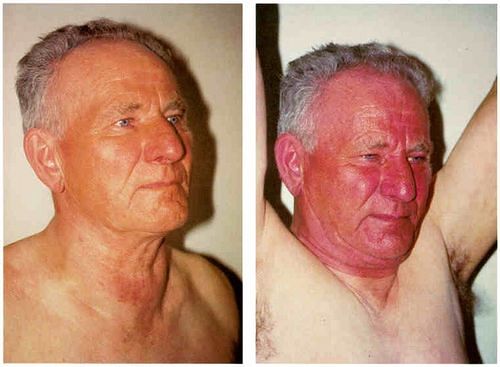
The warmth is often accompanied:
- Persistent flush of the face
- Redness of the elbows
- Palmar erythema
Hyperpigmentation
- Both localized and generalized distribution
- Due to increased release of pituitary adrenocorticotropic hormone compensating for accelerated cortisol degradation
- Jellinek’s sign: Hyperpigmented eyelids
Pruritus
- Generalized
- With or without urticaria
Due to Goitre
- Pemberton’s sign: Facial suffusion provoked in a large substernal goitre
- Maroni sign: Erythema (sometimes with pruritus) may occur in the skin overlying a toxic goitre
Hair Changes
- Scalp hair may be fine and soft
- May be accompanied by a diffuse nonscarring alopecia.
- L-Triiodothyronine was shown to stimulate proliferation of outer root sheath keratinocytes and dermal papilla cells
- Hypertrichosis
- May be related to alterations in the proteoglycans associated with dermal papilla
- Sometimes an early symptom of hyperthyroidism is loss of pigment and early gray hair development
Nail Changes
- Shiny, soft and friable
- Onycholysis: Distal separation of the nail from the nail bed
- Plummer’s nails: Concave contour accompanied by distal onycholysis
In Grave’s Disease
- Pretibial myxedema
- Thyroid acropachy
- Scleromyxedema
Pretibial myxedema (Thyroid Dermopathy)
Diffuse or circumscribed mucinous dermopathy
Misnomer: can arise in the hands, arms, shoulders, ankles, feet, ears, face, surgical scars, skin grafts, animal bites
Typically bilateral, asymmetric, firm, nonpitting, and painless nodules and plaques present on the extensor aspects of the lower legs and feet
3 clinical variants of thyroid dermopathy:
- Sharply circumscribed (Nodular + Tuberous lesions in shins and toes)
- Diffuse (Solid, non-pitting edema of shins and feet)
- Elephantiasic (Edema + Nodule)
Nodules are pink or skin-coloured, sometimes yellow-brown and waxy, with prominent hair follicles giving a ‘peaud’orange’ appearance
Mechanism: Circulating IgG stimulating glycosoaminoglycan production in fibroblasts and in keratinocytes
M/E: Accumulation of glycosoaminoglycans (such as hyaluronic acid and chondroitin sulfate) within the papillary dermis of both affected and normal skin.
Thyroid dermopathy doesn’t necessarily remit after thyroid hormones normalize
Monitoring: skin thickness with USG
Treatment:
- Topical glucocorticoids, with or without occlusive dressings
- Intralesional glucocorticoid injections
- Debulking procedures
- Octreotide
- Plasmapheresis (perhaps acting by removal of TSIs)
- Photochemotherapy
- Intravenous immunoglobulin
- Graduated compression bandaging
Thyroid Acropachy
Triad of digital clubbing, soft tissue swelling of hands and feet, and periosteal new bone formation on the shafts of the phalanges and distal long bones
Asymptomatic and requires no therapy
Pathognomic radiographic osseous change: lamellar periosteal reactions paralleling the daiphyses of the hands and wrists
Scleromyxedema
Numerous firm, white, yellow, or pink papules scattered on the face, trunk, and extremities.
Accumulation of acid mucopolysaccharides, mostly hyaluronic acid, in the dermis, accompanied by large fibrocytes
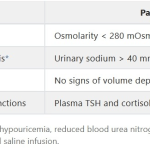
HYPOTHYROIDISM
Causes
- Hashimoto’s thyroiditis
- Iodine deficiency
- Radioactive iodine treatment
- Thyroidectomy
- Medications
- Postpartum
- Subacute thyroiditis
Dry skin (Xerosis)
- Commonest skin manifestation
- Due to change in skin texture & poor hydration of stratum corneum
- Rough and covered with fine scales
- Epidermis is thin & hyperkeratotic, & there is follicular plugging.
- In atopic individuals and keratosis pilaris, findings are more prominent on the extremities in contrast to hypothyroidism where the changes are generalized.
- May affect the development of the lamellar granules (Odland bodies), which are vital in the establishment of a normal stratum corneum
- May be severe enough to develop into icthyosis vulgaris
- Skin is prone to dermatitis (eczema craquelé)
Cold skin
- Reduced core temperature
- Reduced thermogenesis
- Diminished perfusion
- Reflex vasoconstriction compensatory to diminished core temperature
- Demonstrable by nail-fold capillaroscopy
Myxedema
- Generalized myxedema is a classic sign
- Swollen, dry, pale, waxy, and firm to the touch
- Facial features: Puffy with involvement of eyelids, lips, tongue and nose
- Appears pale because of the dermal mucopolysaccharides and dermal water content which alter the refraction of light.
- Mucopolysaccharides appear first in the papillary dermis and are most prominent around hair follicles and vessels.
- Separate the collagen bundles
- Resolve with thyroid hormone replacement
Carotinemia
- Yellowish tinge of palms, soles and nasolabial folds
- Due to accumulation of carotene in stratum corneum
- Occurs due to defective conversion by liver of carotene to vitamin A
Purpura
- Diminished levels of clotting factors
- Loss of vascular support secondary to the dermal mucin
Xanthomatosis
- Secondary to hyperlipidemia
Hypohidrosis
- Decreased eccrine gland secretion
- Glands are atrophic on histologic examination
- Contributes to dryness of skin
- Hypohidrosis, accompanied by diminished epidermal sterol biosynthesis, may lead to acquired palmoplantar keratoderma.
Poor Wound Healing
- Proportional to the degree of hormone deficiency
- Topical thyroid hormone accelerates wound healing
Hair Changes
- Dry, coarse, brittle and slow growing.
- Both patchy and diffuse loss of scalp hair
- Loss of outer third of the eyebrow (madarosis – Hertog’s sign)
- Diminished body hair – Pubic and axillary hair may be sparse
- Massive telogen effluvium may occur when there is abrupt onset of hypothyroidism, and the percentage of scalp hairs in telogen is generally increased in hypothyroid states
- Diminished sebum secretion contributes to the coarse appearance of the hair
- Sometimes, hair loss is the only apparent symptom of hypothyroidism
Nail Changes
- Grow slowly
- Thickened, striated and brittle
- Onycholysis
Candida folliculitis
- Sebaceous glands of hypothyroid patients secrete decreased sebum
- Hair follicles may develop a flora with lipophilic organisms, which are replaced by Candida albicans
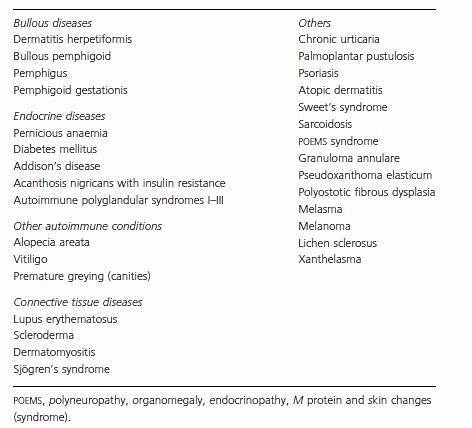
THYROID AUTOIMMUNITY AND SKIN DISEASE
Vitiligo and alopecia areata often precede thyroid dysfunction by many years. Therefore, the presence of elevated
thyroid antibodies may serve as useful clinical tool in euthyroid subjects with vitiligo and alopecia areata to identify patients at risk for thyroid disease.
Possible pathogenesis:
- Immunomodulatory effects of antithyroid antibodies
- Molecular mimicry between thyroid and disease-specific epitopes
- Genetic link between anti-thyroid autoimmunity and the susceptibility to autoimmune disease
THYROID MALIGNANCY
Skin metastasis from a thyroid carcinoma is rarely a presenting feature of an underlying malignancy.
Clinically, the investigation of a flesh coloured skin nodule, particularly in the scalp area, should include the possibility of metastatic thyroid carcinoma.
Metastatic thyroid carcinoma involving the skin can easily be mistaken for a primary adnexal skin tumour.
The correct diagnosis requires a high index of suspicion and the liberal use of immunohistochemical stains.
The development of antibodies against the thyroid transcription factor TTF-1 has provided a useful tool to screen for metastatic carcinomas.
Thyroglobulin expression identifies carcinomas of thyroid follicular cell derivation, including both papillary and follicular types.
Medullary carcinomas are readily identified by neuroendocrine markers, including synaptophysin, chromogranin, and CD56, in addition to the specific tumour marker of this entity, calcitonin.
Presentation prepared by:
Shuvechha Pandey, Srijana Shakya, Sulabh Shrestha
KISTMCTH, Nepal