Table of Contents
Learning Objectives
- List the differential diagnosis for an acutely painful scrotum.
- Understand the anatomical basis of testicular torsion.
- List common presenting signs and symptoms of testicular torsion.
- Describe both initial and definitive management of testicular torsion.
- Explain why torsion is an emergent condition and discuss the time for salvage of the testicle.
Some cases to start with:
- 14 year male presents with testicular pain upon awakening that morning. He has had several episodes of similar pain that resolved spontaneously in the past, but this time the pain is persisting.
- 23 year man complains of three days of painful urination and a swollen testicle.
Acute Scrotum
| Emergent | Non-emergent |
| Testicular torsion | Appendage torsion |
| Fournier’s gangrene | Acute epididymitis |
| Abdominal aortic aneurysm | Testicular/scrotal abscess |
| Traumatic testicular rupture | Testicular cancer with bleeding |
| Peritonitis with patent processus vaginalis | Renal colic |
| Incarcerated inguinal hernia | Hydrocele |
| Varicocele | |
| Henoch-Schonlein Purpura | |
| Orchitis |
By age:
Infant
- Hernia
- Hydrocele
Child
- Hernia
- Torsion
- Epididymitis
Adolescent
- Epididymitis
- Torsion
- Trauma
Adult
- Epididymitis
- Hernia
- Trauma
- Tumor torsion
Commonest causes:
- Responsible for 0.5% of total ED visits.
- 85-90% cases: Appendage torsion + Testicular torsion + Acute epididymitis
- 75% cases: Testicular torsion + Acute epididymitis
- 25% cases: Testicular torsion (1:4000 males; peak age ~14 yrs)
- M/C cause: Acute epididymitis
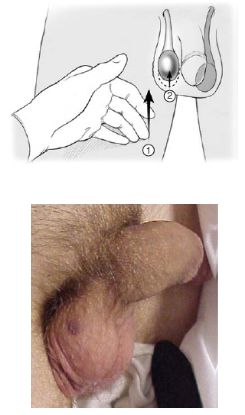
Special signs and Techniques
- Stroking ipsilateral inner thigh – reflex elevation of testicle
- Absence of ipsilateral reflex – think testicular torsion
- Presence – 96% NPV for torsion
2. Prehn’s sign
- Relief of pain with scrotal elevation
- Thought to be positive in epididymitis (not reliable)
3. Blue dot sign
- Infarcted appendage (blue dot) seen through scrotal skin
- Think of appendage torsion
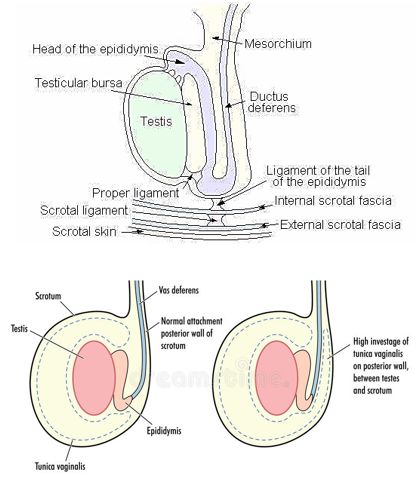
Relevant Anatomy
Normal Testicular fixation in Scrotum:
1.Tunica vaginalis to Scrotal ligament (Gubernaculum)
2.Posterior part of testis (not layered by tunica vaginalis) to scrotum by mesorchium
Increased mobility of testis:
- Defect in normal fixation mechanism
- Long mesorchium
- Exercise or Trauma
- Puberty: Increased weight and vascularity
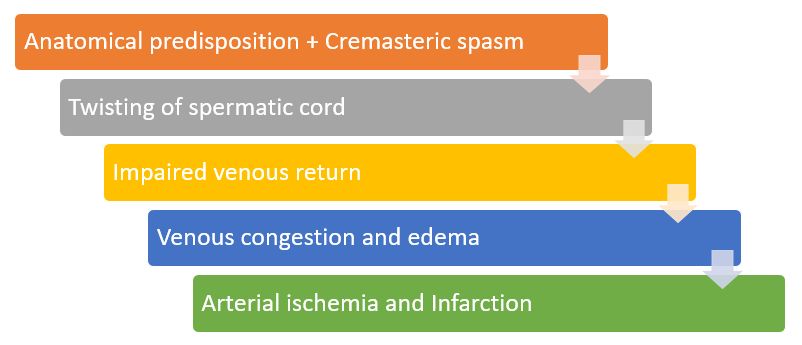
Cremasteric spasm:
Rapid cremaster contraction → elevation +/- rotation of testicle
- Cremaster = Internal oblique muscles
- Inserts into spermatic cord in spiral fashion
- Abdominal muscle contraction = Cremaster contraction
- Association with blunt abdominal trauma and straining
Winter syndrome: During winter when males are in bed
- Scrotum relaxed in warmth → Testicles freely mobile → Testicles twist à Sudden exposure to cold → Contracts quickly → Torsion
Sleep: Strong cremasteric reflex associated with nocturnal erections
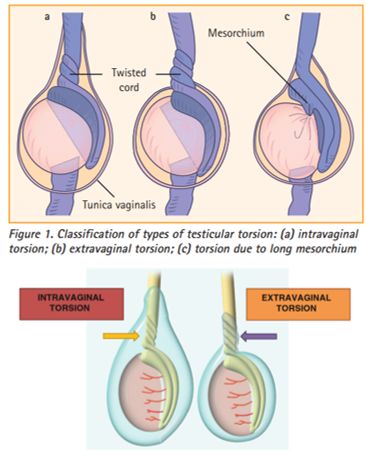
Types of Testicular Torsion
1. Extravaginal (perinatal period)
- Scrotal ligament not developed
- Prenatal = “vanishing” testis
2. Intravaginal (after perinatal period) – more common
- Bell-clapper deformity (in upto 12% asymptomatic men)
- Long mesorchium
Pathophysiology of Testicular Torsion
Mikuz Histologic Grading of Testicular Torsion
| Grade | Features | Time |
| 1 | Intertubular edema, limited blood extravasation, desquamation of germ cells | <4 hours |
| 2 | Diffuse intertubular hemorrhage, focal necrosis of the germ cells | 4-8 hours |
| 3 | Diffuse infarction of parenchyma | >12 hours |
Features Suggestive of Testicular Torsion
- Severe acute testicular pain +/- nausea & vomiting (26-60%)
- Prophetic pain (self-limiting previous episodes)
- Affected testicle lies high up (Deming’s sign; 26-80%)
- Horizontal lie of contralateral testicle (Angell’s sign; 25-90%)
- Anterior position of epididymis rather than posterior
- Absent cremasteric reflex (40-100%)
- Reactive hydrocele (52%); Fever (infarction; 8-41%)
In adolescent boys with lower abdominal pain examine external genitalia to rule out scrotal or testicular pathology. Non-scrotal/abdominal pain accounts for 5-25% cases in cases of acute testicular torsion.
TWIST score
| Finding | Points |
| Testicular swelling | 2 |
| Hard testicle | 2 |
| Absent cremasteric reflex | 1 |
| Nausea or vomiting | 1 |
| High-riding testicle | 1 |
PPV 100% when >5 points (Suggesting stat urological consult)
NPV 100% when <2 points (Suggesting clinical clearance)
Scores from 2-5 patients require U/S for further assessment
Time is Testicle
| Duration | Salvage rate |
| <6 hrs | 90-100% |
| 12-24 hrs | 20-50% |
| >24 hrs | 0-10% |
| Torsion | Infarction onset |
| 3 | 2 hours |
| 1 | 12-24 hours |
| <1 | >24 hours |
Clinically – Complete vs Incomplete? – Difficult to determine
Surgery – reduces pain and other symptoms’ duration
Don’t rely on symptoms duration. All require emergent urologic evaluation.
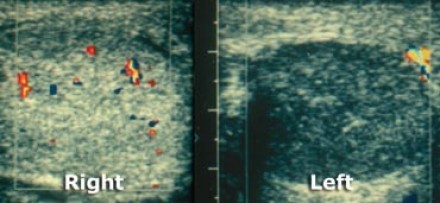
Imaging in Testicular Torsion
Indications:
1.Clinical doubt as to the cause
2.Failure to respond to treatment
Clinical setting of testicular torsion – USG shouldn’t delay intervention
Gold-standard: Color Doppler USG
Uncertain perfusion on color Doppler USG: Nuclear medicine scan
Gray-scale USG
Abnormal spermatic cord twist (Whirlpool sign)
- Sensitivity: 96%
Normal linear cord (In patients without torsion)
- Specificity: 99%
Normal homogenous echo pattern = Viable testis
Hypoechoic/Inhomogenous echo pattern = Non-viable testis
Color Doppler USG
Sensitivity: 96-100%; Specificity: 84%-95%
Incomplete torsion:
- Elevated resistive index (>0.75)
- To-and-fro flow
Complete torsion: Absence of blood flow in testis and epididymis
Nuclear Medicine Scan
Tc-99m Pertechnetate
Sensitivity: 80-90%
Specificity: 90-100%
Early: Nubbin sign (Abrupt cut-off of iliac a.)
Late: Halo/Rim/Dough-not sign
Manual Detorsion of Testis
Steps for manual detorsion of testis in testicular torsion has been discussed here.
Definitive Management of Testicular Torsion
- Surgical detorsion and bilateral orchipexy to the scrotum.
- Contralateral orchipexy is obligatory.
Informed consent prior to surgical exploration:
- Removal or fixation of affected testis depending upon viability
- Fixation of contralateral testis should the diagnosis of torsion prove correct
- Testicular atrophy (upto 68%) even following surgery
- Subfertility – abnormal semen analysis in 50-87%
Answer to the cases we began with:
1. A 14-year-old male presents to ED with complaints of testicular pain upon awakening that morning. He has had several episodes of similar pain that resolved spontaneously in the past, but this time the pain is persisting.
Ans: Testicular torsion
2. A 23-year-old man complains of three days of painful urination and a swollen testicle.
Ans: Epididymo-orchitis
Take Home Messages
Time is Muscle!! (Myocardial infarction)
Time is Brain!! (Stroke)
Time is Testicle!! (Testicular torsion)
Castration by procrastination.
When in doubt, check it out (explore).
MCQs on Testicular Torsion
Comment down the best choices:
1. Regarding testicular torsion, which ONE of the following statements is TRUE?
A. It is mostly due to lateral rotation of the spermatic cord
B. The cremasteric reflex is always absent
C. It can be reliably excluded with scrotal ultrasound scan
D. It can be associated with a fever
2. Testicular torsion of at least _____ degrees is necessary for complete arterial occlusion?
A. 180
B. 360
C. 520
D. 720
3. What is Angell’s sign?
A. High riding contralateral testis
B. Twisted spermatic cord on affected side
C. Horizontal lie of testis on contralateral side
D. Horizontal life of testis on affected side
4. An adult patient presents with recurrent severe testicular pain with spontaneous resolution. Testis was found to have horizontal lie on examination. Urine analyses and culture were normal. Doppler reveals hyper-perfused testis. What is the best management for this patient?
A. Antibiotics
B. Conservative management with scrotal support and analgesia
C. Orchiopexy
D. No treatment needed
References:
Halls GD, Dietrich T, Ford D. Diagnosis and Emergency Department Management of Urologic Emergencies in the Male Patient: Part I [Internet]. AHC Media - Continuing Medical Education Publishing. 2002 [cited 2017Dec30]. Available from: https://www.ahcmedia.com/articles/118262-diagnosis-and-emergency-department-management-of-urologic-emergencies-in-the-male-patient-part-i
Jezek D. Atlas on the Human Testis. 1st ed. London: Springer London; 2013.
Sandler M. Diagnostic nuclear medicine. 1st ed. Philadelphia: Lippincott Williams & Wilkins; 2003.
Salem A, H A. An Illustrated Guide to Pediatric Urology. 1st ed. Switzerland: Springer International; 2017.
King C, Henretig F, Young C. Textbook of Pediatric Emergency Procedures. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2007.
N, O'Flynn KJ, Pearce I. Testicular torsion: a urological emergency. Trends in Urology; Men's Health. 2010; 1(1): 31-4

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.




b
b
c
d
The answers for these MCQs are:
1. d
2. c
3. c
4. c
Explanation for the MCQs:
1. Lateral rotation of spermatic cord – Only 1/3rd cases
Doppler USG has both false positives and negatives
Nausea, vomiting and fever – 20% cases
2. Complete arterial occlusion occurs at 450-540 degrees of rotation. – Ma and Mateer’s emergency Ultrasound (3rd edition)
However complete torsion is defined as ≥360 degrees.
3. In cases of torsion due to long mesorchium. Horizontal position of testicle will not be appreciable in the affected side but will be appreciable on the opposite side. A gap may also be felt between the testis and epididymis.
4. Suggestive of Intermittent testicular torsion. Scrotal orchidopexy proved to be superior to conservative measures in cases of ITT in adults. – Al-Kandari AM, Kehinde EO, Khudair S, Ibrahim H, ElSheemy MS, Shokeir AA. Intermittent Testicular Torsion in Adults: An Overlooked Clinical Condition. Medical Principles and Practice. 2017;26(1):30-34. doi:10.1159/000450887.