Table of Contents
Synonyms: Nervus radialis, Musculospiral nerve
Recommended reading:
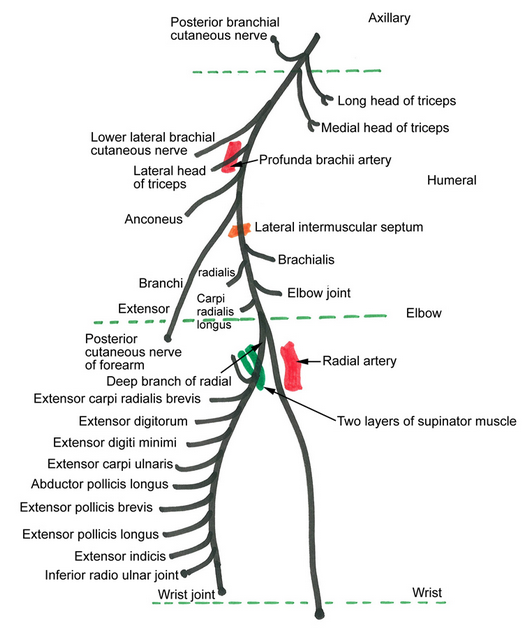
Course
1. Origin: Terminal branch of Posterior cord of brachial plexus (Root value: C5, C6, C7, C8, T1)
2. Posterior axilla: It lies behind the axillary and upper part of the brachial arteries, passing anterior to tendons of subscapularis, lattisimus dorsi and teres major.
3. Triangular interval: Exits axilla via triangular interval or lower triangular space to enter posterior compartment of arm, inferior to brachial artery.
4. Posterior compartment of arm: Descends obliquely from medial to lateral in the spiral (radial) groove along with profunda brachii artery between lateral and medial head of triceps and reaches the lateral border of distal 1/3rd of humerus.
5. Lateral intermuscular septum: Pierces the lateral intermuscular septum ~10 cm proximal to lateral epicondyle to enter the anterior compartment of arm.
6. Anterior compartment of arm: It lies in the muscular groove between brachialis (medially) and brachioradialis (laterally).
7. Hueter’s line (Interepicondylar line): Gives off superficial (sensory) branch 2.5 cm above to 3 cm below the Hueter’s line and deep (motor) branch (roughly around anterior to lateral epicondyle).
8.a. Deep (motor) branch of radial nerve (DBRN) passes through Radial tunnel: Curves around lateral and posterior surface of proximal radius to reach posterior compartment of forearm.
Mnemonic: fromed by FREAS
- Fibrous bands
- Recurrent radial vessels (leash of henry) – radial neck
- ECRB (Extensor Carpi Radialis Brevis)
- Arcade of Frohse (supinator arch – formed by the fibrous band between the 2 heads of supinator) – commonest site of entrapment in radial tunnel syndrome; located 3-5 cm below Hueter’s line
- Supinator (distal border)
8.b. Posterior interosseous nerve (PIN): DBRN emerges as PIN out of the radial tunnel (~7.5 cm distal to the radial head).
- Proximal part of forearm: In the extensor compartment of forearm, it descends between superficial (EDC) and deep (APL) extensor muscle group accompanied by posterior interosseous artery.
- Distal part of forearm: It lies in the interosseous membrane
As it emerges out of supinator, it ramifies into a large number of unnamed branches and it often called “cauda equina” of arm.
9.a. Superficial (sensory) branch of radial nerve (SBRN):
- Proximal forearm: It descends along anterolateral side of forearm. It lies on supinator, pronator teres, flexor digitorum superficialis and flexor pollicis longus, covered by brachioradialis.
- Distal forearm: It emerges posteriorly between brachioradialis and ECRL tendon ~8 cm proximal to radial styloid to become subcutaneous.
- Wrist: It runs as dorsal radial sensory nerve crossing the Anatomical snuff box between EPB and APL, lateral to radial artery.
Innervation by Radial nerve
Motor
a. Above radial groove: Long and Medial head of triceps
b. In radial groove: Lateral and Medial head of triceps, Anconeus
c. Below radial groove and in the radial tunnel: Brachialis, Brachioradialis, ECRL, Supinator, ECRB
d. PIN:
- Superficial: ECU, EDC, EDM
- Deep: APL, EPB, EPL, EIP
Mnemonic: Radial nerve supplies BEAST muscles.
1. Brachialis, Brachioradialis
2. Extensor muscles of the forearm
3. Anconeus
4. Supinator
5. Triceps
Note: Brachialis has dual innervation (median and radial nerve)
Sensory
a. Above radial groove: Posterior cutaneous nerve of arm
b. In radial groove: Lower lateral cutaneous nerve or arm and Posterior cutaneous nerve of forearm
c. Dorsal radial sensory nerve: Wrist, Dorsal lateral 3 and 1/2 fingers upto distal interphalangeal joint and corresponding dorsum of hand
Radial Nerve Injuries and Entrapment
Safe zone of radial nerve in arm:
Upto 10 cm distal to lateral acromion.
Upto 10 cm proximal to lateral epicondyle.
Safe zone for dorsal radial sensory nerve:
An isosceles tringle can be formed taking 3 points, i.e. radial styloid, lister’s tubercle and point of exit of dorsal radial sensory nerve (between ECRL and BR ~8 cm above radial styloid). All the branches of superficial radial nerve is found in the radial half of the triangle. Hence, the region in ulnar half of the traingle is suggested as a “safe zone” for K-wire placement.
With a sound knowledge of radial nerve anatomy, we will know what clinical findings to expect with the different level of radial nerve lesions.
Very high (above spiral groove): Total palsy (BEAST) + Total sensory loss of radial territory including Sensory loss: Over autonomous zone (1st dorsal webspace)
Etiology: Shoulder dislocation, Proximal humerus fracture, Crutch palsy
High: Triceps spared + Posterior sensory of arm spared
- In spiral groove: Loss of sensation over lower lateral arm and posterior forearm
- In distal humerus: Above mentioned sensation are spared
Etiology: Fracture shaft of humerus, Saturday night palsy, Injection, Callus, Torniquet
Low (Below elbow): Brachioradialis (BR), ECRL, ECRB spared
Etiology: Fracture of radial head, Posterior dislocation of radius at elbow joint
Radial tunnel syndrome (RTS): Compression within radial tunnel formed by FREAS as described above. It is associated with pain over lateral forearm and tenderness over “mobile wad” 3-6 cm distal to radial head. Motor dysfunction is usually not a feature. It is also named as treatment resistant tennis elbow.
PIN palsy: No wrist drop, No sensory deficit
Posterior interosseous nerve entrapment: It is always associated with motor dysfunction.
Wrist: Dorsal radial sensory nerve (Wartenberg’s disease or Cheiralgia paresthetica of Handcuff neuropathy)
Wartenberg’s disease: Compression of dorsal radial sensory nerve between Brachioradialis and ECRL in pronation due to scissoring effect. There is tenderness to palpation over the superficial radial nerve.
Mnemonic: E-WTF (Extensors in What The F**k)
1. Very high: Elbow extensors not spared
2. High: Wrist extensors not spared
3. Low: Thumb extensor-abductor not spared, Finger (MCP joint) extensor not spared
Tests for Radial Nerve
Provocative maneuvers for entrapment syndromes
a. Deep radial nerve (PIN) entrapment:
- Proximal wrist pain with resisted wrist extension.
- Extend elbow and pronate arm – resisted supination will lead to RTS symptoms.
- Resisted middle finger extension compresses the PIN against the edge of ECRB, causing pain.
b. Superficial radial nerve entrapment: Forced forearm pronation resproduces symptoms within 1 minute (due to scissoring effect of ECRL and BR).
Motor and Sensory Examination for Radial nerve
To test the muscles, patient is asked to perform the particular muscle function against resistance and examiner palpates for the muscle.
Triceps: Eliminate gravity by placing upper arm parallel to ground. Supporting the limb, ask the patient to further extend the elbow against resistance from half-extended position.
Lateral epicondyle group:
- Brachioradialis: As the patient flexes forearm against resistance in neutral position, brachioradialis is felt in lateral antecubital fossa.
- ECRL and ECRB: Ask the patient to extend and adduct the wrist against resistance with forearm pronate and feel the muscle.
- Supinator: With forearm extended (to minimize role of biceps), patient is asked to resist pronation and muscle is felt.
PIN – superficial group:
- ECU: Patient is asked to extend wrist in ulnar direction against resistance
- EDC: With forearm in neutral position, patient is asked to extend MCP joint with resistance placed just proximal to PIP joint
- EDM: Similar to EDC, but in little finger
PIN – deep group:
- APL: Stabilize hand and ask the patient to extend MCP joint of thumb in radial direction against reistance (i.e. plane of palm).
- EPL: With hand fisted, patient is asked to extend thumb against resistance placed over distal phalanx
- EPB: With hand fisted, patient is asked to exted the thumb against resistance placed over proximal pahalanx
Note: Abductor pollicis brevis (thenar muscle supplied by median nerve) abducts the thumb in a direction perpendicular to plane of palm, i.e. towards the ceiling on a hand laid flat on floor.
References:
- Anatomy and Human Movement E-Book: Structure and function by Roger W. Soames
- Examination of Peripheral Nerve Injuries – An anatomic approach (2nd Edition) by Stephen Russell
- Manual of Peripheral Nerve Surgery – From the basics to Complex procedures (Thieme)
- Trescot, A. M. (Ed.). (2016). Peripheral Nerve Entrapments. doi:10.1007/978-3-319-27482-9

He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.


Wrong information about muscles innervated! Brachialis is supplied by musculocutaneous nerve NOT radial nerve!!!
Hello Vaidehi,
Though the primary innervation of brachialis is from the musculocutaneous nerve, it is one of the muscles with dual innervation. The lateral part is often supplied by the radial nerve. Some studies have found that in around 80% cases, there is dual innervation from musculocutaneous nerve and radial nerve.
Hi My name is Kavitha, my father had an accident and his right hand was seized, doctor said it is brachial damage so we did surgery on him , but it didn’t help, now he was suffering from pain for days….any suggestions is there from ur side sir