A) Epidemiology:
- 2nd commonest fracture around elbow after supracondylar fracture
- Commonest age of occurrence: 5-10 years
- Lateral condylar fracture is common than medial condylar fracture due to 2 reasons:
- Radius articulates with the lateral part of the condyle and therefore the force from sudden impacts is primarily directed laterally.
- Lateral epicondylar ridge is smaller and weaker than its medial counterpart.
- It is the fracture of necessity i.e. needs ORIF
- Most fractures are Type IV Salter Harris fractures
B) Mechanism of Injury:
- Pull-off theory (Jakob): Avulsion of lateral condyle by ECRL and brachioradialis during adduction of supinated forearm
- Push-off theory (Milch): Fall on outstretched hand causes impaction of radial head into the lateral condyle causing fracture
C) Classifications:
a. Milch: Fracture line based –
- Milch Type I: Fracture line lateral to trochelar groove (Salter harris type IV; stable)
- Milch Type II: Fracture line into trochlear groove (Salter harris type II; unstable; more common)
b. Jakob and Weiss: Displacement and articular congruency based –
- Type I: <2mm displacement
- Type II: ≥2mm displacement but intact articular cartilage
- Type III: ≥2mm displacement but associated disruption of the articular surface
Modified Weiss classification: No need for arthrogram
1. Type I: <2 mm displacement
2. Type II: 2-4 mm displacement
3. Type III: >4 mm displacement (displacement of >4 mm correlated with disruption of cartilaginous hinge, shown by arthrogram)
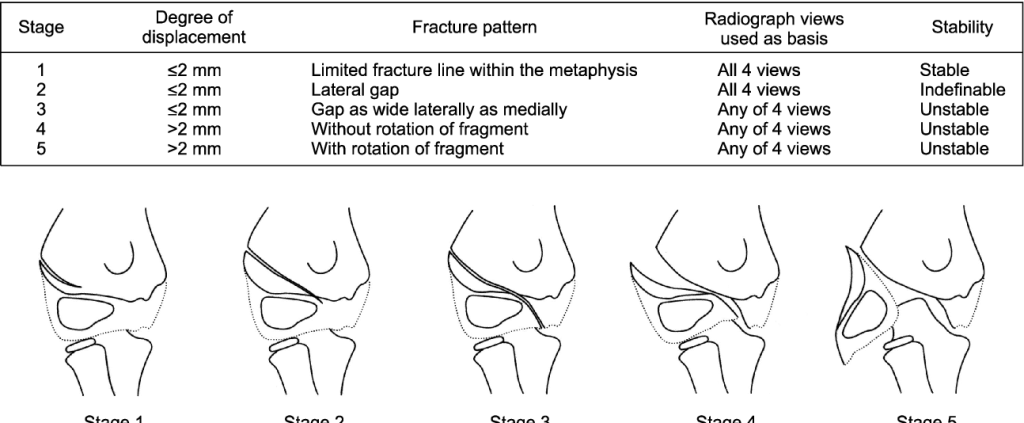
c. Song: Stage of fracture progression based –
| Stage | Degree of Displacement | Fracture pattern | Radiograph views used | Stability |
| 1 | ≤2 mm | Limited fracture line within metaphysis | All 4 views | Stable |
| 2 | ≤2 mm | Lateral gap | All 4 views | Indefinable |
| 3 | ≤2 mm | Gap as wide laterally as medially | Any of 4 views | Unstable |
| 4 | >2 mm | Without rotation of fragment | Any of 4 views | Unstable |
| 5 | >2 mm | With rotation of fragment | Any of 4 views | Unstable |
D) History and Examination:
- Swelling and tenderness over lateral aspect of elbow
- Reluctance to use the arm and resistance to passive motion
- Can lead to minimal swelling and deformity, leading to delayed presentation
- Increased pain with resisted wrist extension/flexion
E) X-ray examination:
- AP and lateral views
- Internal oblique view: detects minimally displaced fracture as the fractured fragment frequently lies posterolaterally
Lateral humeral condyle fracture plane is at a mean of 21+/-2 degrees to the anatomical axis on a lateral radiograph. Therefore, an AP radiograph of the humerus taken at 20 degrees elevation results in a view along the fracture plane and offers a view of maximal displacement of the fracture.
F) Treatment:
1. Weiss type 1, Song 1: Can be managed with long arm cast with forearm in supination and wrist in extension (to relax deforming muscles i.e. extensor-supinator complex)
- Duration: 4-6 weeks
- Follow up: Weekly out of cast X-rays (Internal oblique, AP, lateral and 20 degree AP)
2. Weiss type 2, Song 2-4: Closed reduction and percutaneous fixation can be performed if satisfactory reduction achieved (fracture gap <1-2 mm)
- Surgical Technique for Closed Reduction and Percutaneous Pin… : Techniques in Orthopaedics (lww.com)
- Can use K-wires or Cannulated screws
- Using 2 instead of 3 K-wires when stability is adequately achieved improves range of motion and reduces bone spur formation
3. Weiss type 3, Song 5, failed closed reduction: Open reduction and Internal fixation
- Lateral approach to the pediatric distal humerus (aofoundation.org)
- K-wires, Metaphyseal screw fixation or Transcapitellar screw fixation
- Surgical tips:
- Slight anterior incision to reduce stretch of scar
- Use of a dental mirror to see across the joint surface and confirm reduction.
- Hockey stick arthrotomy in line with the fibres of the lateral radial collateral and annular ligament.
- 20 degrees elevated distal humeral views to confirm reduction of the fracture intraoperatively.
- Avoid dissection of the posterior aspect of the lateral condyle as this will result in damage to the only blood supply to the capitellum.
- Lateral epicondylar artery (from radial collateral artery) and branch from medial collateral artery both enter posteriorly and anastomose.
K-wire configuration: 1.6 or 2 mm K-wires
1st K-wire: From center of capitellum, parallel to the joint line and advance to medial part of trochlea (to hold the joint surface aligned)
2nd K-wire: Inserted behind the first K-wire and advanced proximally along the lateral column of the humerus as far as the anterior cortex.
There should be atleast 60 degrees divergence between K-wires.
K-wires should have posterior to anterior angle on lateral view.
G) Complications:
- Reduced range of motion
- Avascular necrosis (AVN)/fish tail deformity: as a result of posterior dissection
- Non-union/Malunion: due to wide fracture displacement due to constant extensor pull
- May lead to cubitus valgus deformity (due to undergrowth of lateral condyle) and tardy ulnar nerve palsy
- Cubitus valgus deformity is treated with wedge osteotomy if the angle is more than 20 degrees
- Tardy ulnar nerve palsy: Ulnar nerve palsy seen after several years resulting from friction neuritis (after stretching) due to valgus deformity. It is treated with anterior interposition of the ulnar nerve.
- Lateral overgrowth/prominence: sometimes, overgrowth of lateral condyle may occur due to overstimulation of lateral growth plate and parents should be counselled about this in advance; this may lead to cubitus varus (gunstock deformity)
- Pin tract infections
References:
- Stevenson, R. A., & Perry, D. C. (2018). Paediatric lateral condyle fractures of the distal humerus. Orthopaedics and Trauma. doi:10.1016/j.mporth.2018.07.013
- Martins T, Marappa-Ganeshan R. Pediatric Lateral Humeral Condyle Fractures. [Updated 2022 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560664/